Transitional Year Residency Program
A Message from the Program Director
Thank you for your interest in the Nuvance Health Transitional Year Residency Program.
Our Transitional Year residents work closely alongside residents in Internal Medicine, Surgery, Family Medicine and Emergency residency programs. All residents complete standard core rotations in surgery, medicine, ICU & ER to develop broad medical knowledge and patient care skills.
We are proud of our commitment to medical education and offer our Transitional Year residents hands-on training in a productive, well-balanced learning environment. Wellness is a top priority, and our program is designed to prioritize an excellent educational and clinical experience while supporting a healthy working atmosphere. We believe in a collaborative approach that fosters collegiality within our program, and with our sponsoring and partner residency programs. Our dedicated faculty, from a variety of specialties, provide support and mentorship to our residents as they progress toward the next stages of their training.
Following their time in our program, residents go on to pursue training in anesthesiology, diagnostic radiology, physical medicine and rehabilitation, and more. Our program has a close partnership with the Anesthesiology and Neurology Residency Program, with 11 of our 15 intern positions reserved for their PGY2/CA-1 slots.
We hope you’ll consider joining us here in the beautiful Mid-Hudson Valley!

Sanjay Thomas, MD
Director, Transitional Year Residency Program

Christina Boyce
Program Manager, Transitional Year
Program Structure
The primary purpose of Transitional Year residency training is to provide residents with a well-balanced educational program covering multiple clinical disciplines. Training is designed to facilitate preparation for a specific specialty, including specialties requiring a year of fundamental clinical education as a prerequisite. This program is 13 (4 week) blocks in length. The Transitional Year Residency Program functions under the sponsorship of the Nuvance Health General Surgery Residency Program and Internal Medicine Residency Program.
During Transitional Year residency training at Nuvance Health, each resident is expected to develop strong clinical skills in a program that emphasizes experience in multiple clinical disciplines; experience includes, at a minimum, 24 weeks in Fundamental Clinical Skills rotations. Residents must demonstrate proficiency in comprehensive patient evaluation, assessment and reporting skills. To be assigned progressive responsibility for the management of specific patients, residents must also develop differential diagnosis and test interpretation skills.
During Nuvance Health’s Transitional Year Residency Program, the Program Director will:
- Adjust each resident’s schedule based on the requirements of the advanced standing program (PGY2) to which each Nuvance Health resident is matched.
- Customize each resident’s block schedule, procedure requirements, and evaluation schedule to meet the requirements of the resident’s future specialty.
- Ensure that unmatched residents receive a comparable opportunity to modify their training year, and discuss this modification with the resident, considering each individual’s educational and career goals and priorities.
- Maintain contact with each appropriate PGY2 program director.
- Send updated resident status and progress reports to the PGY2 program director at least twice annually, or as required by the PGY2 advanced standing ACGME RC requirements.
- Transfer all required documents, summative evaluations and records to the advanced standing program within 60 days after the resident graduates from the Transitional Year Residency Program.
Residents rotate monthly through a diverse curriculum of general surgery and internal medicine rotations, and gain experience in emergency medicine, ambulatory care and at least two months of electives of their choice. Various elective options are provided to residents, including anesthesiology, neurology, research, surgery and surgery subspecialties, pulmonary medicine, obstetrics and gynecology, radiology and any other rotation discussed and agreed upon in conjunction with the Transitional Year Residency Program Director.
Residents are also required to complete a month in ambulatory medicine and may choose between an internal medicine or general surgery ambulatory clinic. Resident training takes place at Vassar Brothers Medical Center (VBMC) in Poughkeepsie, NY, or Northern Dutchess Hospital (NDH) in Rhinebeck, NY.
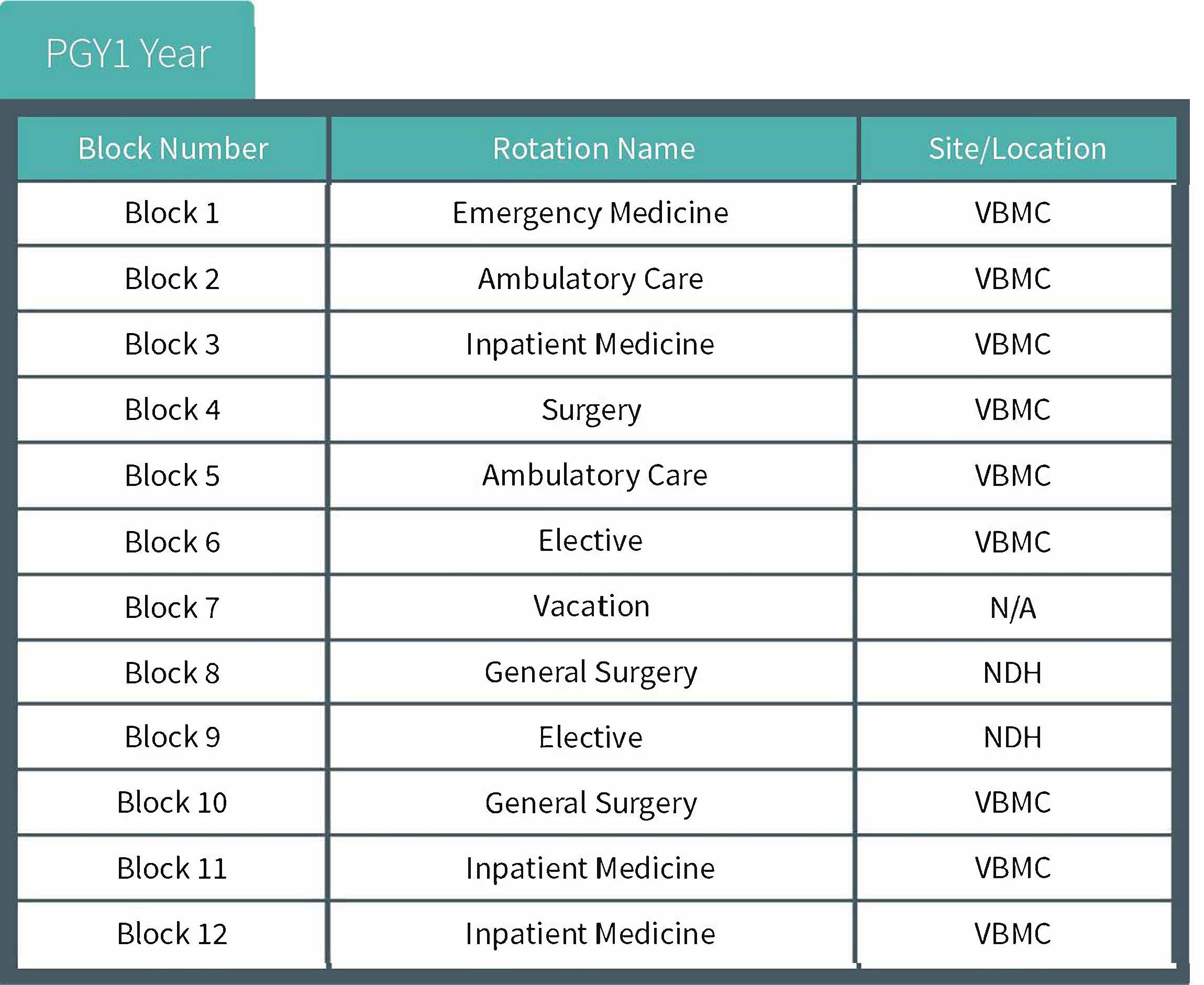
An example of one resident’s training in this program is shown below. This is only an example and may be adjusted by the Program Director to ensure adequate experience and ACGME compliance.
Additional Program Offerings
Orientation – As a new Transitional Year resident, you will participate in a two-week new intern orientation prior to beginning in the program on July 1. This will help you adjust to residency life and provide you with an overview of programs, topics and required information. Non-patient care/medical knowledge curriculum topics are covered as well, including interpersonal communication skills, professionalism, systems-based practice and practice-based learning and improvements.
Academic Didactic Schedule
All Transitional Year residents are expected to participate in didactic and conference sessions for the specialties in which they rotate. The weekly Transitional Year didactic session is facilitated by the Program Director and is attended by all Transitional Year residents not on Fundamental Clinical Skills rotation. Sessions are hosted at Vassar Brothers Medical Center, and serve as a regularly scheduled touch-point for all residents in the program to discuss their progress, challenges and goals.
Research Opportunities
The Transitional Year Residency Program requires that all residents participate in scholarly activity and ensures sufficient opportunity for research and academic participation is made available to all. On an annual basis, residents are provided with exposure to evidence-based medical research and review skills, methodologies and professional resources. Topics include the following:
- Healthcare policy and administration
- Critical analysis of medical literature
- Use and utility of various statistical methodologies
- Research structures and methodologies
- Application of evidence-based medicine in practice
- Leading quality, performance improvement and patient safety initiatives
During orientation, residents are given the research curriculum, which outlines the scholarly activity requirements for completion of the program:
- Each resident must complete one form of scholarly activity under faculty member supervision, which may include:
- Completing an abstract/poster
- Initiating a team-based quality improvement (QI) project
- Submitting or publishing an article in a peer-reviewed journal
- This scholarly activity may be the result of the required QI project, independent study or clinical case observation.
The Program Director meets quarterly with each resident to review the research requirements and the individual’s research progress. These reviews are focused on ensuring the resident is familiar with the requirements and is aware of the resources and support available to be successful.
Residents then each select a topic to be approved by the Program Director for a research project. Residents work with a faculty member (preferably their mentor) and other residents, if applicable, to design a study, receive proper Institutional Review Board (IRB) approval, conduct the research project and develop a presentation or publication for submission to a relevant source (conference or journal). The assigned faculty member provides guidance during this process by evaluating and approving each step of the study.
Additionally, residents have access to Nuvance Health’s quality improvement and research departments for support in their scholarly pursuits. Scholarly activities and quality improvement initiatives at Nuvance Health are designed to help residents advance their knowledge in the principles of research and become competent in evidence-based medicine through self-directed assessment and learning. After completing research projects, residents present their findings at the Annual Resident Research Day sponsored by Nuvance Health, or at a local, regional or national conference. Residents may also submit their findings to a relevant peer-reviewed journal for publication considerations.
How to Apply
The Nuvance Health Transitional Year Residency Program thanks you for your interest in applying to our program. We accept all applications through ERAS only and participate annually in the NRMP Match Program.
Due to the impact of the pandemic, all interviews for academic year 2023-2024 will be held virtually.
If you wish to apply to our Anesthesiology Residency Program as an advance standing candidate, that information can be found here.
The following items are required for consideration for an interview. All items must be received through the ERAS application portal:
– Proof of U.S. medical school graduation
– USMLE or COMLEX scores
– MSPE (Dean’s) letter
– Three (3) letters of recommendation
– Personal statement
– Current CV
International Medical Graduates:
The Transitional Year Residency program accepts applications from foreign nationals who are holders of a Green Card (permanent resident) only.
We interview candidates on select dates in October, November, December and January. These dates are provided to select residency applications via ERAS invitation. Other important dates include:
Mid-September: NRMP registration opens
Late October: MSPE (Dean’s) letters released through NRMP
Late November: Standard registration deadline for applicants
Late February: Rank order list deadline
Mid-March: Match week
Mid-March: Email notification of “You’ve Matched”
Mid-March: MATCH DAY CELEBRATION
Requirements
The following items are required for consideration for an interview. All items must be received through the ERAS application portal:
- Proof of U.S. medical school graduation
- USMLE or COMLEX scores
- MSPE (Dean’s) letter
- Three (3) letters of recommendation
- Personal statement
- Current CV
International Medical Graduates:
The Transitional Year Residency program accepts applications from foreign nationals who are holders of a Green Card (permanent resident) only.
Important Dates
We interview candidates on select dates in October, November, December and January. These dates are provided to select residency applications via ERAS invitation. Other important dates include:
- Mid-September: NRMP registration opens
- Late October: MSPE (Dean’s) letters released through NRMP
- Late November: Standard registration deadline for applicants
- Late February: Rank order list deadline
- Mid-March: Match week
- Mid-March: Email notification of “You’ve Matched”
- Mid-March: MATCH DAY CELEBRATION
Frequently Asked Questions
Thank you for your interest in the Nuvance Health Transitional Year Residency Program! If you need more information, please contact us.
Where will I train?
The majority of training takes place at Vassar Brothers Medical Center in Poughkeepsie, NY, with some rotations occurring at Northern Dutchess Hospital in Rhinebeck, NY. The ambulatory clinic experience occurs at a Ambulatory Surgery Center or inpatient medicine clinics. Some specialty experiences and electives, if selected, may occur at any of these locations.
When is my application due?
Applications are due through ERAS on November 30.
How many residency positions are there?
We accept 15 residents each year. We want our community to be tight-knit, and all residents to feel they are an important part of the program, while providing an excellent educational experience. We accept only PGY1 positions. Six of those positions are pre-allocated for Nuvance Health Anesthesiology and five are reserved for the Nuvance Health Neurology categorical positions
When are the interviews?
Interviews take place on select dates in October, November, December and January. If you are selected for an interview, you will be notified via ERAS.
