General Surgery Residency Program at Vassar Brothers Medical Center

Message from the Program Director
The Nuvance Health General Surgery Residency Program at Vassar Brothers Medical Center offers a residency training program with a very robust exposure to a high volume of routine surgical care, and also highly complex surgical care with subspecialty trained faculty. Although most of our residents choose to pursue fellowship training, our program also prepares residents to enter directly into general surgery practice. The most special aspect of our residency program is that we offer exposure to a high volume of complex surgery in a smaller, highly capable hospital with a more personable community setting than is typically seen in most academic medical centers. In addition to routine general surgery care, our program offers exposure to:
- Level 2 Trauma Surgery, and acute care surgery program
- Minimally invasive laparoscopic and robotic surgery
- Bariatric Surgery
- Comprehensive surgical oncology services with dedicated surgeon-led teams in breast, gastrointestinal, liver/pancreas, thoracic, head/neck, melanoma and gynecologic oncology
- High-volume hepatobiliary and pancreatic services including minimally invasive hepatobiliary surgery
- Hyperthermic intraperitoneal chemotherapy (HIPEC), and isolated limb infusion (ILI). Vassar may be one of the only community-based hospitals to offer both of these services
- High quality breast surgery program including reconstruction
- Progressive endovascular and open vascular surgery
- Comprehensive cardiac surgery program
- Multidisciplinary wound management and hyperbaric program
In 2021, Vassar Brothers Medical Center opened a new 750,000 square-foot patient pavilion including 15 new operating room (OR) suites, an innovative conference center and private rooms for an enhanced patient care and educational experience.
Our dedicated faculty is energetic, engaged and passionate about teaching clinical excellence. Our goal is to maintain a collegial environment, making resident wellness a priority while emphasizing patient care. We understand that a modern, strong, comprehensive residency training program needs to work in concert with efforts to maintain resident health and well-being. Each resident is matched with a faculty mentor, with a 1:1 faculty-to-resident ratio. There is a strong support system to ensure residents are part of the family at Nuvance Health.
With the exception of a fellowship in breast surgery, we do not have any other surgical fellows. As such, teaching efforts and operative exposure are dedicated to our resident staff.
We are seeking good people with the potential to be great physicians, and well-rounded surgeons and clinicians. In your search for a residency program, we can offer opportunities to structure training in pursuit of career paths in community-based general surgery, academic settings and specialized fellowship training. All residents engage in scholarly activity, focusing on research, quality improvement and outcomes-based practice.
We take pride in our clinical performance, our facilities and our training program, and we are extremely thankful for the great community we have at Nuvance Health. We hope you’ll consider joining us.
Dr. James Nitzkorski, MD, FACS, FSSO
Attending Surgical Oncologist
Program Director, General Surgery Residency Program
 For questions or more information, contact Program Manager, Maggie Forte margaret.forte@nuvancehealth.org or (845) 790-1311
For questions or more information, contact Program Manager, Maggie Forte margaret.forte@nuvancehealth.org or (845) 790-1311
Statement on Diversity
The Department of Surgery at Nuvance Health – Vassar Brothers Medical Center is committed to fostering a culture that reflects the incredibly rich diversity of our community and of the patients we treat. The Department of Surgery welcomes individuals of all backgrounds, cultures and individual differences regardless of ethnicity, gender, race, religion or sexual orientation.
We are committed to inclusion, and we believe that a diverse academic community enhances our ability to treat our patients and train our medical students and residents.
Nuvance Health is Joining Northwell Health

https://www.northwell.edu/nuvancehealth
Nuvance Health is proudly joining Northwell, one of the largest health systems in the Northeast. This means you and your family will have expanded access to renowned care, resources and expertise—through the 13,500 providers, more than 1,000 care locations and 28 hospitals throughout Northwell.
Northwell and Nuvance Health have a unified goal: Transform health care and build a healthier future for the residents of Connecticut and New York.
Northwell will become the sponsoring institution for all Nuvance residency and fellowship programs. While we are still finalizing the timeline for the full transition, all programs currently remain part of the Nuvance Health Consortium.
Nuvance and its residency and fellowship programs will become part of a designated region within Northwell, maintaining the existing model of regional oversight for GME programs.
Northwell strongly values GME, and being part of this network will provide our residents with access to enhanced educational resources and opportunities.
No major changes in the surgical residency program is expected in terms of hospital sites or rotations.
Program Structure
First Year:
First-year trainees spend the entire year at Vassar Brothers Medical Center. Each resident functions as a member of the surgical team. PGY-1 residents are responsible for patient care on the floors and participate in surgical care in the operating room. Each PGY-1 resident typically participates in between 100-150 cases during the intern year.
Rotations during the intern year include general surgery/colorectal surgery, acute care/trauma, surgical oncology, vascular surgery, and the intensive care unit.
Second Year:
PGY-2 residents spend their year at Vassar Brothers Medical Center, except for one month spent at New York Presbyterian on the pediatric surgery service. PGY-2 residents develop increasing amounts of conditional independence and gain experience in providing surgical consultation services in the emergency department and on the patient care floors. Rotations during the PGY-2 year include vascular surgery, general surgery/colorectal surgery, acute care/trauma surgery, endoscopy, breast surgery, palliative care, and intensive care. PGY-2 residents also begin to develop more comfort with robotic surgery, both at the bedside and on the console.
Third Year:
PGY-3 residents transition to being senior residents and become team leaders during some rotations. Surgical experience is deepened, and residents spend Four months on the surgical oncology service with a deep exposure to complex patients and operations. PGY-3 residents also rotate on the vascular service, breast surgery, general surgery, and they do one month on the head/neck surgery service. PGY-3 residents also rotate again at New York Presbyterian on the liver transplant service.
Fourth Year:
PGY-4 residents experience ongoing conditional independence and become supervising physicians for more junior residents. The year is operative heavy, and residents have an opportunity to spend time on an elective (at Vassar Brothers, or elsewhere). PGY-4 residents rotate on thoracic surgery, general surgery/colorectal surgery, acute care surgery/trauma, and spend time at Northern Dutchess Hospital on the bariatric surgery service. PGY-4 residents spend one month at Cooper University in Camden, NJ for a deep immersive trauma surgery experience. PGY-4 and PGY-5 residents evenly split the “Chief Call” roll while on-call.
Fifth Year:
Chief residents are expected to master their leadership skills, and further refine their operative technique with ongoing exposure to both routine and complex cases. Chief residents run the service, supervise, and teach junior residents and medical students, and have important roles in quality improvement and program leadership. Chief residents typically graduate with 1200-1400 cases.
Core Rotations at Vassar Brothers Medical Center
Blue Team
-General Surgery
-Robotic Surgery
-Colorectal Surgery
Green Team
-Surgical Oncology
-Hepatobiliary + Pancreatic Surgery
-Breast Surgery
-Head/Neck Surgery
-Reconstructive Surgery
Orange Team
-Trauma Surgery
-Acute Care Surgery (ACS)
-Surgical Critical Care
Red Team
-Vascular Surgery
-Thoracic Surgery (non-cardiac)
Training Sites
Vassar Brothers Medical Center (VBMC) – Poughkeepsie, NY

Our residency is based at Vassar Brothers Medical Center which is a 365 bed Medical Center located in the Mid-Hudson Valley region of New York State. Nearly all time is spent at VBMC. Residents are exposed to a high volume of both routine and complex operations.
Rotations include General Surgery, MIS & Robotics, Colorectal Surgery, Trauma, Critical Care, Acute Care Surgery and Consultation, Surgical Oncology (Liver/Pancreas, GI, Melanoma), Head/Neck including reconstructive surgery and free flaps, Breast Surgery, Vascular Surgery, Thoracic Surgery, Endoscopy, Palliative Care
Northern Dutchess Hospital (NDH) – Rhinebeck, NY

-Northern Dutchess Hospital is home to the Bariatric Surgery Program. Rhinebeck is a short drive from Vassar Brothers Medical Center.
New York-Presbyterian/Columbia University Medical Center – New York, NY

-PGY-2 residents spend one month on the Pediatric Surgery Service (housing is provided)
-PGY-3 residents spend one month on the Liver Transplant Service (housing is provided)
Cooper University – Camden, NJ

-PGY-4 residents spend one month one month on the Level 1 Trauma Surgery service. This rotation supplements our level 2 Trauma Surgery experience at Vassar Brothers with a deep immersive trauma surgery experience. Residents are exposed to a large volume of penetrating volume at Cooper. Housing is provided.
Academic Offerings
Residents’ Journal Club
As a first step in learning how to effectively practice evidence-based medicine, interns and residents participate in Journal Club to appraise a recent study published in the medical literature.
Boot Camp
As a new resident, you will participate in an intern boot camp during your first week here. This will help you adjust to residency life and provide you with an overview of programs, topics and required information. Non-patient care/medical knowledge SCORE Curriculum topics are covered as well, including interpersonal communication skills, professionalism, systems-based practice, and practice-based learning and improvements.
ABSITE In-Training Exam
Residents’ medical knowledge and clinical reasoning will be benchmarked for measuring longitudinal growth through the results of the annual American Board of Surgery In-Training Exam. All general surgery residents will complete the exam. Results will be reviewed with the program director to inform discussions and individualization of curriculum and clinical training (e.g., reading material, board prep and electives).
Academic Half Day

Most didactic experience occurs on Thursday mornings. Residents enjoy protected time to focus on the educational aspects of residency. Mandatory conferences are held regularly in the Nuvance Health General Surgery Residency Program.
All lectures are designed to provide residents with a broad range of knowledge on the ACGME competencies. We use the SCORE Curriculum, and we also provide our residents access to True Learn, and other supplemental resource for academic support.
M&M
Weekly, 7 am Thursdays
SCORE
Weekly, 8 am Thursdays. SCORE provides residents and training programs with high-quality educational materials and a structured program for self-learning. SCORE focuses on all areas of general surgery. All surgical residents have access to the entire SCORE program which includes
- More than 470 module topics covering all six competency areas in general surgery
- This Week in SCORE (TWIS) – a topic of the week program
- Chapters from 15 leading surgical textbooks
- 2400+ multiple-choice questions for resident self-assessment
- 230+ narrated operative videos
- 170+ SCORE School webinars
- 80+ anatomical illustrations
Film Club
Monthly, Thursdays. Surgical videos are reviewed to provide a deep level breakdown of surgical technique, higher-level concepts, and intra-operative decision making in small group sessions. Film club is a small group resident teaching session moderated by a small number of faculty.
Multidisciplinary Tumor Conference
Surgical residents are encouraged to attend tumor conferences. Residents rotating on the breast surgery service routinely present the patients they have encountered during clinic.
Breast
Thoracic
Rectal/GI
Head/Neck
Urologic
Grand Rounds
Monthly topics cover a wide range of medical and surgical subjects.
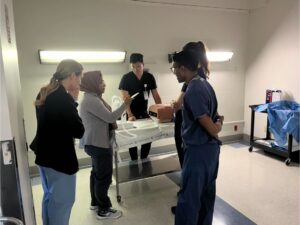
Simulation
A variety of simulation exercises occur throughout the year and cover topics such as Trauma resuscitation, vascular anastomotic lab, laparoscopic skill, robotic simulation.
Robotic Certification
Residents who intend to use robotic surgery as a part of their practice are encouraged to complete DaVinci certification before leaving residency. The residency program will assist residents in obtaining DaVinci certification.
Schwartz Rounds
Quarterly, system-wide conference dedicated to wellness. Recent topics included “Nurturing Resilience in Ourselves and Others” and “Injustice and Bias in Healthcare.”
Palliative Care

We became one of the first residency programs in the country to make a structured palliative care experience part of the surgical residency curriculum, with a one-month dedicated rotation in palliative care medicine during the PGY-2 year. The rotation includes a deep simulation workshop with standardized patients designed to improve the ability for our residents to break bad news, and also disclose inadvertent events in a safe, simulated environment.
Wellness

Residents who are well make excellent physicians. The importance of wellness is emphasized throughout the residency program. Some of the things we have done to promote wellness:
- Peloton exercise bike located in the Surgical Resident Call Room
- Strict adherence to 80 hour work-week (plus NYS duty hour restrictions)
- Annual welcome party for incoming residents
- Newly refurbished Call Room space
- Collegial and mutually respectful atmosphere
- Access to mental health and employee assistance program
- Anonymous program feedback options
- Faculty “open door” policy
- Residency-sponsored events such as
- Hiking and Axe throwing event
- Apple picking

- Resident-Only Gym installed (located within VBMC) with free weights, rack, yoga mats, treadmill, elliptical machine.

Fifth Thursday Program
When a “5th Thursday” of the month occurs, residents are dismissed immediately following didactic sessions. Residents are encouraged to use the time for wellness activities and attend personal appointments such as primary care visits, etc.
Surgical PA Program
Vassar Brothers Medical Center has a large surgical PA program. Our surgical PAs are embedded into general surgery teams and rotate into the call schedule to help maintain patient care and to de-emphasize use of residents for “service” related tasks. Our surgical PAs help us maintain the educational focus of the residency program.
Call
Overnight call is variable, depending on rotation and personnel but is typically no more frequent than q4, and can be as favorable as q6.
Residents as Teachers and Leaders Course
We send all of our senior residents to take this immersive course at the American College of Surgeons in Chicago each year. The goal of this course is to help surgery residents develop some of the essential nonclinical skills that will be critical to their success as senior-level residents and practicing surgeons. The course faculty are nationally renowned clinical and educational professionals who will provide an interactive learning environment. Residents learn to lead a team more effectively, resolve conflict, be better teachers, give constructive feedback, and apply these skills during and after residency.
Curriculum Design
Curriculum Design
Feedback from residents has been critical to our success so far. Our residents meet with our Faculty and Program Director frequently to review our program, and changes have been made to optimize the quality of the educational program at VBMC.
For example, new changes for the 2023/2024 academic year the VBMC residency program include:
- A formal PGY-2 rotation in Palliative Care, making VBMC one of the only surgical training sites in America to designate a formal palliative care rotation.
- A formal PGY-4 rotation in Trauma Surgery was established at Cooper University (housing provided) to supplement our Level-2 trauma experience at VBMC.
Research and Quality Improvement Opportunities
Kyle J. Thompson, PhD – Director of Surgical Research
In 2024, the Department welcomed Dr. Kyle J. Thompson, PhD. Dr. Thompson’s early work focused on the impact of obesity as a risk factor for hepatocellular carcinoma. More recently, Dr. Thompson served as a senior data scientist at the Carolinas Center for Surgical Outcomes Science before joining Nuvance Health.
Dr. Thompson holds regular office hours in the GME Suite at Vassar Brothers Medical Center to assist residents and faculty with research projects.



Clinical Trials
- Breast Cancer Clinical Trials
- Colorectal Cancer Clinical Trials
- Melanoma Clinical Trials
- Lung Cancer Clinical Trials
- Genetic Cancer Clinical Trials
- Gynecology/Oncology Cancer Trials
Residents have access to a quality assurance officer who assists in the development and implementation of all quality improvement projects. In addition to each resident’s project mentor, the quality assurance officer serves as an excellent resource for residents to use when working on quality improvement projects and implementation or analysis.
Residents are also supported by the quality assurance team committee at each training location. This experience provides residents with the ability to see quality assurance and improvement issues and solutions from a hospital perspective.
Residents are also provided with access to NSQIP, a surgical de-identified registry of all procedural cases that compares data between teaching hospitals across the nation. This serves as another great resource for residents to find data and conduct robust clinical research. This data is stored on a cloud-based library. In addition to NSQIP, residents have access to registries such as VQI and STS.
Operative Experience
Operative Experience:
Early and Robust operative experience with proper supervision and teaching is emphasized.
Interns typically log between 100-150 cases during their first year in the residency, and some have logged over 200 case during the PGY-1 year. Our Chief residents have an incredible operative experience, and graduates tend to log between 1200-1400 cases.
Our Department has only one fellow in breast surgery, who spends about half of the year at Danbury Hospital. As such, the clinical experience at Vassar Brothers Medical Center is focused entirely on centering the educational experience around our residents without competition for clinical experiences.
As an example, based on case log data some of our residents have been in the 95 percentile nationally for liver and pancreas operations.
Simulation and Robotics
Each resident is experienced in simulation at Nuvance Health.



In 2024, a new Simulation Center was opened in the resident space in Vassar Brothers Medical Center.
The DaVinci Robotic Skills Simulator is available to residents for extra training including off-hour/weekend access so that residents may practice while on-call. The Robotic Curriculum ensures that each resident develop proficiency in surgical robotics early in residency training. Once basic and bedside proficiency is gained, residents begin work on our dual-console robotic platform. Our goal is to assure that each resident is ready for a robotic practice upon graduation.
In addition to robotic and laparoscopic simulation experiences, the Surgical Residency Program at Vassar Brothers has a formal endoscopy curriculum and periodic workshops. Some recent workshops have included:
- Vascular anastomosis workshop
- Skin closure workshop
- Airway procedures
- Robotic day
- Intra-operative fluorescence workshop
- Surgical Stapling workshop
In addition to simulation options at Vassar Brothers Medical Center, The Harold A. Spratt Center for Simulation and Clinical Learning is a state-of-the-art facility located at Danbury Hospital. VBMC residents have access to this center.
Highlights of the Center
Between the space at Vassar Brothers and Danbury Hospital, residents have access to features including, but not limited to:
- Flexibility to replicate alternative clinical environments, such as outpatient exam rooms
- Control rooms isolated from the lab space to allow remote control of simulators and audio/ visual equipment
- One-way glass to allow learners a sense of independence while maintaining direct supervision by faculty
- Networking to support the integration of the highest tech simulation equipment available
- Functioning hospital gas panels with oxygen, air and suction
- A monitor to display vital signs and data pertinent to a simulation scenario
- High-fidelity manikins that simulate human physiology and pathology
- Ddebriefing rooms for instruction and discussions
- Cutting-edge audio/visual capability so scenarios can be recorded and played back for analysis while debriefing and data can be captured for research or assessment
- A standardized patient program that uses live people trained to act through clinical scenarios
- Educational and technical support from a specialized simulation team to ensure well-executed and effective utilization of simulation modalities
Teaching
Nuvance Health – Vassar Brothers Medical Center (VBMC) surgical residents have important teaching roles for medical students. We are a primary teaching site for third- and fourth-year students at the Touro College of Medicine, and we routinely welcome visiting medical students to our services.
In addition to teaching medical students, PGY1 residents from the VBMC Transitional Year Residency (Blue, Green) and the Emergency Medicine Residency (Trauma) rotate through the Department of Surgery.
Teaching
Nuvance Health – Vassar Brothers Medical Center (VBMC) surgical residents have important teaching roles for medical students. We are a primary teaching site for third- and fourth-year students at the Touro College of Medicine, and we routinely welcome visiting medical students to our services.
In addition to teaching medical students, PGY1 residents from the VBMC Transitional Year Residency (Blue, Green) and the Emergency Medicine Residency (Trauma) rotate through the Department of Surgery.
How to Apply
How to Apply
We accept all applications through the ERAS only and participate annually in the NRMP Match Program.
Individual requests for personal review outside of ERAS are not considered by the residency program, and the program will not reply to unsolicited emails from applicants outside of ERAS system.
Interview Requirements
The following items are required for interview consideration. All items must be received through the ERAS application portal:
- Personal statement
- CV
- Three (3) letters of recommendation
- USMLE Step 1 or COMLEX-1 pass.
- USMLE Step 2 or COMPLEX-2 CS score
- MSPE (Dean’s) letter
Interviews
For the 2024/2025 academic year, interviews will be virtual. Once an invitation to interview is released, applicants will have 48 hours to accept or decline the interview date. Applicants with unanswered invitations after 48 hours will have their interview invitation withdrawn.
H2 Visas are not supported.
Second Look
An optional, on-site second look date will be announced during interviews. The rank list will be completed prior to the second look date, so the decision to attend will not alter a rank list position.
