Internal Medicine Residency Program at Vassar Brothers Medical Center
A message from the Program Director
I am honored to be the program director of the Nuvance Health Internal Medicine Residency Program at Vassar Brothers Medical Center (VBMC) where everything we do is driven by our focus on two things—excellence in education and phenomenal patient care.
Here at Nuvance Health – VBMC, you have the best of both worlds. We are a young program whose inaugural class started in July 2019. Our first class of 25 graduated together in June 2022 and all of our graduates have gone on to wonderful job opportunities and fellowships. As a newer program, we have been able to build a residency culture from the beginning to meet the needs of modern-day medicine while incorporating techniques to improve resident wellness and work-life balance. We are imaginative and creative, and actively seek out feedback from our residents to help shape and continuously improve the program. However, we also understand that a strong and stable educational structure is essential to allow you to reach your full potential. We have incorporated the best of seasoned programs with the ingenuity and agility of the new, which has helped us adapt to challenges like the pandemic and come out stronger together.
Your education is our priority. We understand that there is a great deal to learn in these three years, and we want your time best spent on mastering your clinical and diagnostic skills, communicating with patients, and learning about systems-based practice. Our curriculum, faculty, resources, and diverse patient population provide an ideal environment for residency training. We are fortunate to have a dedicated, knowledgeable, and easily accessible faculty and staff who are committed to your success. Residents have protected educational time each weekday with a fantastic noon conference series, afternoon report, subspecialty small-group sessions and ambulatory academic half-days.
We have a wide range of medical pathology comparable to most busy academic medical centers but in a community hospital environment, which makes the residency experience appropriately challenging but also enjoyable. All of the inpatient rotations are at VBMC in Poughkeepsie, New York. VBMC is a busy, 350-bed tertiary care facility with 66 ER beds, 30 ICU beds, an average case mix index of 1.76, 2,000 average monthly discharges, and 58k yearly emergency department visits. We have support services from all medicine subspecialties and perform advanced procedures onsite including TAVR, ECMO, EBUS, PCI, etc.
We require all residents to participate in scholarly activity. During their tenure here, the 25-resident graduating class of 2023 had 173 case report abstracts accepted for presentation at international, national, and local conferences (including ACP, NYACP, SGIM, NYRIF/CCR, CHEST, ACC, ATS, ACG, ASCO, Endo Society) and had research abstracts (9) and case abstracts (23) accepted for publication in peer reviewed journals. Our graduates have gone on to fellowships at extremely busy academic medical centers where they have been selected as chief fellow, won awards at national conferences, and been hired to stay on as faculty.
We want our trainees to graduate with the preparation and confidence to pursue any of the diverse careers a residency in internal medicine allows, whether it is in primary care, subspecialty fellowship or hospitalist medicine. Our established advising program begins early in the intern year to give you the support and resources you need to pursue your goals.
We hope that when you graduate, that you stay here and join our medical community, but we want you to reach your fullest potential wherever it may be and are happy to support you to get there. I hope you will apply to the Nuvance Health Internal Medicine Residency Program at Vassar Brothers Medical Center. You will gain the professional experience you need and the personal connections you want while enjoying the beauty of the Hudson Valley.
Sincerely,
Susan Collins, MD, FACP
Program Director, Nuvance Health VBMC Internal Medicine Residency
Associate Designated Institutional Official, Nuvance Health West
Program Structure
As an ACGME-accredited internal medicine residency program, our curriculum and clinical training experiences will prepare graduates to be not only independent practitioners or candidates for fellowship training, but also leaders in the field of medicine. By graduation, all residents will receive approximately the same exposure listed below in terms of weeks. The structure allows residents to develop a solid foundation in internal medicine with the flexibility to tailor your experiences as a second- and third-year resident to prepare you best for your future career choice.
PGY1
| 10-11 weeks | Ambulatory Medicine |
| 2-6 weeks | Medical Step-down Unit |
| 12-13 weeks | Inpatient Medicine |
| 4-6 weeks | Night Medicine |
| 8-10 weeks | ICU |
| 4 weeks | ER |
| 2 weeks | Ambulatory Selective |
| 2 weeks | Elective |
| 4 weeks | Vacation |
PGY2
| 10-11 weeks | Ambulatory Medicine |
| 8-10 weeks | Inpatient Medicine |
| 2-4 weeks | Inpatient Cardiology |
| 4-6 weeks | Night Medicine |
| 4-6 weeks | ICU |
| 2 weeks | Geriatrics |
| 2 weeks | Neurology |
| 2 weeks | Outpatient Hematology/Oncology |
| 10-12 weeks | Elective |
| 4 weeks | Vacation |
PGY3
| 10-11 weeks | Ambulatory Medicine |
| 2-4 weeks | Medical Step-down Unit |
| 2 weeks | Jr. Hospitalist (Graduated Responsibility Inpatient Training aka GRIT) |
| 2 weeks | Jr. Primary Care Physician (Graduated Responsibility Outpatient Training aka GROT) |
| 4-6 weeks | Day Admitter/antibiotic Stewardship |
| 4-6 weeks | Medical Admitting Resident/Consults |
| 4-6 weeks | ICU |
| 4-6 weeks | Night Medicine |
| 10-12 weeks | Elective (including option to do 3 weeks of dedicated Point-of-Care Ultrasound training) |
| 4 weeks | Vacation |
The 4+1 Schedule
The Nuvance Health Categorical Internal Medicine Residency Program structure is a three-year program in which our residents usually spend 4 weeks on a given assignment (for example medicine wards or ICU), then one full week in the ambulatory setting which includes dedicated continuity clinic time to see an assigned patient panel. This 4+1 structure allows the resident to focus on learning from the rotation they are on at the time and gives protected time to the ambulatory experience to develop longitudinal relationships with patients.
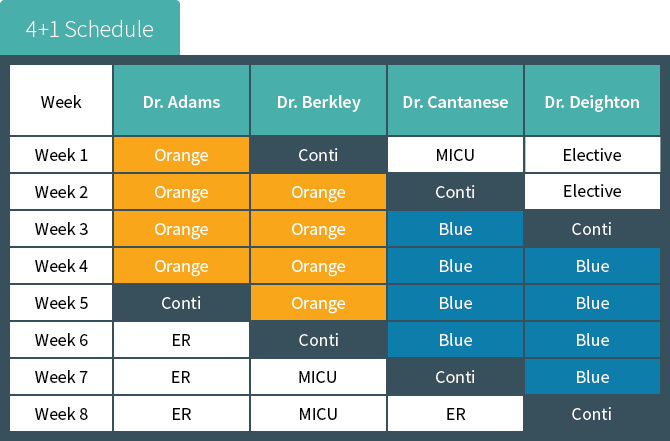
In the above example, Dr. Adams begins his academic year with a four-week rotation on the inpatient medicine orange team. When the fourth week is over, Dr. Adams spends one week rotating in the
continuity clinic and in various other internal medicine subspecialty clinics. Dr. Adams then changes to the next rotation, emergency medicine.
Note that as Dr. Adams is leaving the continuity clinic week, Dr. Berkley is coming into her continuity clinic week; and the pattern continues with Dr. Catanese and Dr. Deighton. These four individuals together comprise the continuity clinic “firm.”
Firms are an additional benefit to our program’s structure. Each firm’s cohort of residents acts as practice partners for one another, mimicking the structure of most private group practices. This real-world experience reinforces the skills and competencies required to be fully prepared to successfully practice medicine by the end of training. The Academic Practice Faculty are dedicated solely to the education of our residents and precepting their patients.
Our goal is to give our residents exposure to all the subspecialties with which a well-rounded primary care physician should be familiar. We have asked our subspecialty faculty to make sure that during the rotations the residents become familiar with common medical conditions in their field but also learn to identify the “red flag” things that would trigger a consult to a specialist on either a routine or urgent basis. In addition to seeing their own panel of patients in the Academic Practice, our interns spend time during the ambulatory week rotating through other medical and non-medical subspecialties to help inform their practice as primary care physicians (ie ophthalmology, physical therapy, infectious disease, etc). Our second- and third-year residents continue to manage their own panel of patients and establish an additional outpatient continuity clinic site either in a medicine subspecialty practice of their choosing or at another primary care site. Also, they have protected time during their ambulatory weeks to design, develop and implement their required scholarly project.
The Ambulatory Experience
Ambulatory Activities:
| Activity | Session(s) | Location |
| Continuity Clinic | 4-5 | P.C. Poughkeepsie Primary Care or Castle Point VA |
| Panel Management | 1 | P.C. Poughkeepsie Primary Care or Castle Point VA |
| Specialty Clinic* | 3 | Ophthalmology, Wound Care, Physical Therapy |
| Academic Half Day | 1 | VBMC |
*PGY2s and PGY3s have one specialty session in an area of their choosing and 3 sessions for participation in scholarly activities in lieu of the 4 specialty clinic sessions when on ambulatory week, whereas PGY1s half one session dedicated to quality improvement skill development.
Continuity Clinic
P.C. Poughkeepsie Primary Care, a Nuvance Medical Practice, is one of the continuity clinic sites for all our residents and is conveniently located adjacent to Vassar Brothers Medical Center. It is a fully academic primary care practice that serves a diverse population of patients in terms of demographics,
socioeconomic status, ethnicity, language, and payer mix. At this office, every patient is scheduled to see a resident, great steps are taken to ensure continuity in patient care when scheduling appointments, and the wait time for appointments is very short. Residents are encouraged to provide high value, high quality care and routinely perform appropriate ambulatory procedures for their panel of patients such as pelvic and breast exams as well as urgent procedures such as incisions and drainages, injections, and more. There is great emphasis placed on the importance of preventive medicine, patient education, communication skills, and patient and resident satisfaction. At this site, residents participate in in-office and telemedicine visits and second- and third-year residents take turns providing after-hours phone call coverage for patients of this office.
The other continuity clinic site is located in the Castle Point Veterans Affairs Hospital. The population of patients at this site tends to be older and more likely to be of male sex then our other continuity site; however, the APD for Ambulatory Education and Medical Director of the Poughkeepsie practice coordinates with the faculty of the VA to ensure the experience is comparable as residents are assigned to one or the other location based on their preferences and availabilities and not both. It should be noted, that second-year residents who have continuity clinic at the VA will spend one half-day per week in the Poughkeepsie office seeing patients with same day visits, those that require procedures, and those who need pre-operative or hospital discharge follow up visits.
Continuity is a key principle to successful patient care and, as such, we go to great lengths to ensure the patients are scheduled for their resident primary care providers for routine visits; however, residents are not always available to address their ambulatory patient’s needs. To ensure continuity in coverage, each resident is assigned to a firm of residents who provide coverage for unexpected patient issues that arise between regularly scheduled visits such as tasks and urgent appointments. Residents regularly communicate with members of their firm in-person and via our EMR to ensure their patients receive the best care no matter what rotation on which they are currently rotating.
Ambulatory Firms
Continuity is a key principle to successful patient care and, as such, we go to great lengths to ensure the patients are scheduled for their resident primary care providers for routine visits; however, residents are not always available to address their ambulatory patient’s needs. To ensure continuity in coverage, each resident is assigned to a firm of residents who provide coverage for unexpected patient issues that arise between regularly scheduled visits such as tasks and urgent appointments. Residents regularly communicate with members of their firm in-person and via our EMR to ensure their patients receive the best care no matter what rotation on which they are currently rotating.
Specialty Clinic
Residents participate in high-yield specialty experiences guided by expert attending specialist providers throughout the Nuvance Health network. While these experiences are assigned to interns, residents have the opportunity to choose their area of specialty in order to provide additional, focused training congruent with their future career goals. Interns will spend 4 half-days of their ambulatory week at the Ophthalmology, Wound Care and Physical Therapy offices. Second- and third-year residents will spend a half day in a specialty office during their ambulatory weeks. The APD for Ambulatory Education will assign them to a specific office based on their preferences and availabilities as well as the availabilities of the offices.
Panel Management
Panel management is a proactive approach to healthcare delivery that aims to ensure that all patients of a given care team receive the necessary preventive services and chronic disease management they deserve, not just those who present for office visits. During the ambulatory week, each resident is given one session (during which they are not scheduled for patient visits) to review their panel of patients, conduct necessary outreach, and plan for in-reach at upcoming visits in order to provide better coordinated care, remain informed and engaged in their patients’ health, improve patients’ clinic outcomes while reducing healthcare costs, and increasing the promotion of preventive medicine by closing care gaps identified. Patients and their resident primary care providers are encouraged to regularly communicate with each other via the patient portal.
Graduated Resident Outpatient Training (GROT)
All PGY3s, regardless of continuity site assignment, will spend 2 weeks at P.C. Poughkeepsie in a mandatory, advanced ambulatory training experience. Each morning (except for Wednesdays), participating residents will see 6-8 patients with acute complaints or need urgent preoperative evaluations or hospital discharge follow ups with a dedicated nurse and attending preceptor in order to mimic independent, private practice. In the afternoons, participating residents will have the opportunity to perform ambulatory procedures, shadow our nursing and case management staff, learn and practice billing and coding principles, and co-precept with the attending staff the interns as they see their continuity patients in order to practice and obtain feedback on their academic and administrative skills.
Ambulatory Academic Half Day
Every Wednesday morning, residents on ambulatory week gather to participate in the Ambulatory Academic Half Day, which includes dedicated workshops, simulations, didactics, and case reviews. The designation of this time to educational endeavors ensures our residents get the highest quality education without the burden of conflicting responsibilities such as patient care and task completion. The weekly sessions include a workshop or simulation exercise, a didactic discussion, and participation in a case-based discussion of high-yield topics in ambulatory medicine as outlined in the Yale Curriculum under a central theme. For example, in the Men’s Health Academic Half Day, residents participate in a simulation exercise regarding the correct performance of external male genital and rectal exams using our life-size full manikin simulator, a case-based discussion of common men’s health issues (such as erectile dysfunction, low testosterone, and benign prostatic, hypertrophy), and complete the corresponding Yale Curriculum modules. During the Diabetes Ambulatory Academic Half Day, residents participate in a workshop designed to teach them how to perform finger stick glucose measurements and administer insulin (using actual glucometers, insulin pens, and other supplies), discuss the American Diabetic Association guidelines for the pharmacologic treatment of type 2 diabetes guided by representative MKSAP questions, and complete the corresponding Yale Curriculum modules.
Conference Curriculum
Inpatient Medicine Afternoon Report
Afternoon Report is a case-based conference which allows residents and faculty to discuss patient care in an organized and efficient manner. Residents present cases to their peers and faculty with a faculty member as the facilitator. The facilitator uses the information in the resident’s presentation as a springboard for robust conversation and discussion to develop medical knowledge and critical thinking skills with a focus on evidence-based practice and high-value care. Interns and residents have separate afternoon report conferences to focus on level-appropriate aspects of diagnosis and management. Resident report is Monday and Intern report is every Friday while the resident is on medicine wards. Board review is done every Wednesday afternoon for residents on the wards where a resident is assigned to put board review questions into a fun “Jeopardy” game format.
Subspecialty Teaching
On Tuesday and Thursday mornings during inpatient wards, the ward team meets in small groups of around 6 residents with a subspecialist attending who does a small group “chalk talk.” This is a revolving curriculum so that by the end of residency all the residents have participated in these sessions. These sessions not only allow the residents to learn skills best taught in such an environment like interpretation of EKGs or understanding non-invasive ventilation options, but it also gives you unique access to subspecialty attendings which naturally fosters collegiality and mentorship which is essential for collaboration in the future on scholarly activity or possibly fellowship pursuit. Current subspecialty teaching sessions include GI, cardiology, pulmonary, ID and rapid response team training. It is a wonderful opportunity – it is not unusual to see a BIPAP machine being wheeled down the hall by the pulmonologist to have the residents learn how to set it up and what the mask feels like.
Noon Conference Series
Our Internal Medicine Noon Conference Curriculum is the core of our academic and didactic series. It occurs Monday thru Friday each week. Taught by board-certified internists and subspecialists, the curriculum is designed to provide residents with a wealth of topics and cases that span the care continuum. We have introduced the ACP Board Review Curriculum as the backbone of our didactics for academic year 2023-2024. We integrate didactics as well as team-based learning exercises to try and meet the needs of our learners. To maximize the experience, Dr. Collins sends out a weekly email with the noon conference topics for the following week along with the recommended reading either from primary articles, review articles or from NEJM Resident 360. At the end of the week, she assigns board review questions from NEJM Knowledge+ to solidify the concepts that were covered. Other regular conferences include high-value care, health care disparities, the business of medicine, career development, resident as teacher and wellness.
Internal Medicine Grand Rounds
Grand Rounds conference is a platform for faculty and invited speakers to present on a variety of topics, including case-based presentations, research, or current relevant topics in the field of Internal Medicine. Grand Rounds occurs monthly during noon conference.
Serious event analysis (SEA)
Serious event analysis/Quality and Process Improvement, formerly Mortality and Morbidity (M&M), occur monthly and are presented by residents with a faculty mentors’ guidance. They are joint conferences with critical care as well as other specialties. Topics are decided by residents and faculty based on actual patient care cases where a significant system error occurred. SEA provides a forum for resident interaction and discussion with attending physicians regarding care that could have been improved, and the opportunity to identify system errors. The faculty mentors facilitate the discussion based on the topic with a focus on approach to root cause analysis.
Residents’ Journal Club
As a first step in learning how to effectively practice evidence-based medicine, interns and residents participate in a weekly Journal Club to appraise a recent study published in the medical literature. Each intern presents at least once at Journal Club. They partner with a subspecialist/internist for development of the topic review and with our Associate Program Director, Dr. Valerie Cluzet, to critically appraise the study, and then presents the appraisal to their peers and faculty during noon conference.
Board Review
Board review is incorporated into noon conference as part of the ACP curriculum as well as into weekly medical knowledge “Jeopardy” games on Wednesday afternoons. Additionally, residents are provided with access to NEJM Knowledge+ and have a generous stipend to reimburse board review materials of their choosing. Topic-based quizzes are assigned weekly to emphasize and practice board-type questions. Ambulatory groups compete with each other to complete the most quizzes for the month and are rewarded when they “win”.
Nuvance Health Residency Joint Program Lecture Series
The lecture series covers GME-wide topics such as resident fatigue, burnout, resident wellness and other issues. Sessions will be hosted by the GME office and invited speakers will present. Topics include, but are not limited to:
- Fatigue
- Stress and depression
- Substance abuse
- Disruptive behavior
- Burnout
- Boundary violations
- Impairment
- Instructive feedback
ABIM In-Service Training Exam
Residents’ medical knowledge and clinical reasoning is benchmarked for measuring longitudinal growth through the results of the annual American Board of Internal Medicine In-Service Training Examination. All internal medicine residents complete the exam annually. Results are reviewed individually with the program director to inform discussions and individualization of curriculum and clinical training (e.g., reading material, board prep and electives). Struggling learners work closely with program leadership to improve study habits and test taking skills so that their confidence improves over the three years well in advance of the actual board exam.
Academic Half Day
Every Wednesday morning, residents on ambulatory week gather to participate in the Ambulatory Academic Half Day, which includes dedicated workshops, simulations, didactics, and case reviews. See Ambulatory Experience tab for further details.
Point-of-Care Ultrasound (POCUS)
In response to overwhelmingly positive feedback from our residents about the POCUS elective, we have added it as a 3-week elective rotation for all our interested third-year residents. POCUS education is supplemented by monthly didactics in our noon conference series and through practical application during patient care.
Research and Quality Improvement Opportunities
The goal of the internal medicine scholarly activity curriculum is to advance each resident’s knowledge of the basic principles of epidemiology and clinical research, including how it is conducted, evaluated, explained to patients, and applied to patient care. Understanding and appraisal of the medical literature is critical to providing evidence-based care. All residents in the Nuvance Health Internal Medicine Residency Program are provided opportunity for, and are fully supported in scholarly activity, including research, quality improvement (QI) and medical education pursuits.
We require each resident to complete scholarly activity and protected time is allotted during ambulatory weeks to work on the projects for the duration of the residency. There is a point system whereby points are earned based on the type of activity and 10 points are required to graduate.
Examples of scholarly activity include research publications, case reports or case abstracts, internal quality improvement projects, teaching presentations, etc. Additional participation by residents above the minimum requirements are highly encouraged. Dr. Valerie Cluzet, Associate Program Director, mentors all residents in the development and conduct of scholarly activity projects that reflect each resident’s interests and career goals. In addition to having dedicated time during ambulatory, additional elective time available. Rotation-specific curriculum is provided to residents with goals and objectives, requirements, and expectations for the rotation.
In addition to individual scholarly projects, all residents will participate in a QI curriculum. Residents, starting in PGY1 year, will work with core faculty to design and implement a QI project, along with the guidance from Associate Program Directors, Dr. Valerie Cluzet and Dr. Becky Mazurkiewicz.
During their residency, the 25 resident class of 2022 completed 6 research projects published in peer-reviewed journals, 9 research abstracts accepted for presentation, 27 case reports accepted for publication in peer reviewed journals and 106 case report abstracts accepted for presentation at international, national, and local conferences, along with 13 ongoing QI projects and 9 IRB-approved research projects.
Application Process
The Nuvance Health Internal Medicine Residency Program at Vassar Brothers Medical Center (ACGME 1403500932, NRMP# 2183140C0) thanks you for your interest in applying to our program. We are an ACGME accredited internal medicine residency program. We accept all applications through the ERAS only and participate annually in the NRMP Match Program. We hope you choose to join us.
For the 2023 ERAS® cycle, our program will be participating in the supplemental ERAS application offered through the AAMC’s ERAS program. Applicants will be required to complete the MyERAS application, and participation in the supplemental ERAS application is optional.
Requirements: The following items are required for consideration of interview. All items must be received through ERAS application portal:
- Personal Statement
- Current CV
- 3 Letters of Recommendation
- USMLE Step 1 Pass or COMLEX Level 1 Score
- USMLE Step 2 CK or COMLEX Level 2 CE Score
- MSPE (Dean’s) Letter
Timeline: We will interview candidates during select dates in November, December and January. Exact dates will be provided to the invited residency applicants via email notification.
Please note, New York State has a 12-week rule for graduates from a non-LCME-accredited medical school regarding limiting the number of required clerkships during medical school that are performed outside of the country of training. See https://www.op.nysed.gov/professions/physicians/license-requirements for further information.
Interviewing
After reviewing applications in ERAS we will send out invites via e-mail with available dates for interviewing. All interviews will be done virtually for the 2023 interview season.
What to expect for the interview day? We do our interviews via Thalamus. You will meet with Dr. Susan Collins the Program Director for an overview of the program and you will have two interviews with faculty members. You will also spend time with our program managers learning more about the area and the benefits of training at Vassar Brothers Medical Center. Most importantly, you will spend time with our current residents in breakout sessions where you can ask them all about the area, the program and why they chose to train here.
Post-interview communication: We are available for any questions that may arise after your interview day. Please free to reach out to the program managers, Nancy Hebrank, Alexandra Belmonte or Kecia Edwards at VBMCIMRecruitment@nuvancehealth.org and to the chief residents at VBMCInternalMedicineChiefs@nuvancehealth.org if you have any lingering questions during this often chaotic time. Please do not feel obligated in any way to provide a thank you note to any of our faculty. Our policy is to not provide any communication to you regarding ranking or fit or preference.
Wellness
We have our own internal medicine residency wellness committee which has a dedicated budget to support wellness activities. Previously our residents have participated in team building activities such as, mini-golfing, bowling, painting night, Lego building competitions and so much more. We have an annual resident wellness retreat. We incorporate wellness into many of our daily activities including guided meditation and gratitude sessions. We have monthly noon conferences dedicated to wellness and organized by the wellness committee leadership.
We also ensure that our residents average weekly duty hours are well under 80 hours by creating a schedule and admitting cap to allow residents adequate time off to focus on developing a work-life balance.
Our Graduates
Class of 2023
Palliative Care Fellowship at the University of Texas in San Antonio, Texas
Hospitalist at Presbyterian Hospital in Albuquerque, New Mexico
Infectious Disease Fellowship at Ohio State University in Columbus, Ohio
4th Year Chief at Northeast Georgia Medical Center in Gainesville, Georgia
Locum Hospitalist at Ochsner Medical Center- Kenner in Kenner, Louisiana
Hospitalist at Norman Regional HealthPlex in Norman, Oklahoma
Hospitalist at SSM Health DePaul Hospital in Bridgeton Missouri,
Cardiac Hospitalist at Christiana Care Health System in Wilmington, Delaware,
Rheumatology Fellowship at Geisinger Commonwealth School of Medicine in Danville, Pennsylvania,
Hospice and Palliative Care Fellowship in San Antonio, Texas,
Hospitalist at Presbyterian Center in Santa Fe, New Mexico,
Primary Care Physician at Kaiser Permanente in Woodbridge, Virginia,
Endocrinology Fellowship at Penn State University in University Park, Pennsylvania
Primary Care Physician in Nuvance Health, Hyde Park, NY
Pulmonary/Critical Care Fellowship at Nuvance Health/Vassar Brothers Medical Center in Poughkeepsie, New York
Hospitalist at Nuvance Health/Vassar Brothers Medical Center in Poughkeepsie, New York
Palliative Care at the University of Missouri Health Care in Columbia, Missouri
Primary Care at Nuvance Health in New Canaan, Connecticut,
Hospice & Palliative Medicine Fellowship at Stony Brook University Hospital in Stony Brook, New York,
Hospitalist at Hartford Hospital in Hartford, Connecticut,
Hospitalist at Memorial Hermann Health System in Houston, Texas,
Nocturnist at Nuvance Health/Danbury Hospital in Danbury, Connecticut,
Hospitalist at ThedaCare in Appleton, Wisconsin
Advanced Fellowship in Cardiovascular Imaging at the University of Florida Gainesville in Gainesville, Florida
Class of 2022
Academic Hospitalist and Core Faculty at Northeast Georgia Medical Center, GA
PGY4 Chief Resident, Nuvance Health, Vassar Brothers Medical Center, Poughkeepsie, NY followed by Clinical Instructor of Medicine at Harvard Medical School / Associate Physician at Brigham and Women’s Hospital / Medical Oncology Hospitalist at Dana Farber Cancer Institute
Core Faculty in ambulatory medicine at WellStar Internal Medicine Residency Program, Atlanta, GA
Endocrinology Diabetes & Metabolism Fellowship at UMass Baystate, Springfield, MA
Hospitalist at Garnet Health Medical Center, Middletown NY
Hospitalist at Guthrie Robert Packer Hospital, PA
Hospitalist at Long Island Jewish Forest Hills, Long Island, NY
Hospitalist at Medstar Georgetown University Hospital in Washington, DC
Hospitalist at Nuvance Health, Vassar Brothers Medical Center, Poughkeepsie, NY (2)
Hospitalist at NYU Long Island Community Hospital, NY
Hospitalist at St. Luke’s University Hospital, Bethlehem, PA
Hospitalist at Washington University School of Medicine, St. Louis, MO
Infectious Disease Fellowship at Dartmouth-Hitchcock Medical Center, NH
Infectious Disease Fellowship at Rutgers New Jersey Medical School, Newark, NJ
Medical Genetics Fellowship at University of California San Diego, CA
Medical Oncology Fellowship at East Tennessee State University, TN
Nephrology Fellowship at George Washington University Hospital in Washington, DC (2)
Nephrology Fellowship at MedStar Georgetown University Hospital in Washington, DC
Primary Care, Swedish Health, WA
Pulmonary and Critical Care Fellowship, Albany Medical Center, Albany, NY
Pulmonary and Critical Care Medicine Fellowship at Louisiana State University School of Medicine, New Orleans, LA
Rheumatology Fellowship at Albany Medical Center, Albany, NY
Rheumatology Fellowship at Houston Methodist, Houston, TX
Our Mission
Our overall two main drivers are to provide phenomenal patient care and to pursue excellence in education. As a program our aim is to build better health for our community by training leaders in the delivery of high quality, compassionate healthcare for a community rich in cultural, economic, gender, racial and physical diversity.
Fast Facts
PROGRAM HIGHLIGHTS
- A “4+1” training model that allows residents to spend one week fully dedicated to continuity of care for their primary care patients in between four-week blocks assigned to a given rotation
- Team-based training with direct patient care and progressive responsibility as residents advance through the program
- Diverse training program with specialty experiences in neurology, critical care, cardiology, endocrinology, pulmonary medicine, geriatrics, rheumatology, point-of-care ultrasound, palliative care and more.
- Daily didactic training exploring topics such as basic sciences, clinical practice, medical ethics and research methods
- Committed, passionate, diverse faculty
- A mentorship program to facilitate professional and personal growth and provide support throughout training
- All residents participate in scholarly activity and/or quality improvement projects
- Emphasis on resident well being
During the first year of training interns care for patients in the emergency department, ICU and medical floors at Vassar Brothers Medical Center, a large tertiary care facility with high patient acuity. They will also be introduced to the Academic Practice where they will provide care for their own panel of patients with their precepting attending faculty. They will work directly with a co-intern, a senior resident and attending physician. Each intern will present at journal club.
During the second year of training, residents will gain experience leading the medical team under the close supervision of their attending physician as they have progressively more independence. Rotations in geriatrics, neurology and outpatient hematology/oncology as well as ample elective time give residents the opportunity to grow their breadth and depth of knowledge tailored towards their future career goals. Residents will design, develop and start to implement their scholarly project.
During the third year of training, residents will gain progressive independence and will solidify their clinical knowledge in more challenging roles with triage and consults developing leadership skills and increased patient care responsibilities. Third-year residents take the lead on cases, and will act as clinicians, leaders and teachers. Third-year residents will also have several elective opportunities to guide their own training path and prepare for the next stage of their career.
FAQs
Why should I come to the Hudson Valley for residency?
It’s beautiful here! It is lovely to enjoy four seasons with apple-picking and hiking with brilliant, colorful foliage in the fall; skiing, sledding, snowboarding and ice skating in the winter; more kayaking and biking in the spring, and enjoying swimming, outdoor concerts, drive-in movie theaters, water parks and more in the summer. We have fantastic restaurants with the Culinary Institute of America 10 minutes away from the hospital and we benefit from a lot of their graduates settling locally. We have multiple local colleges and universities which provide an array of cultural opportunities – the initial Hamilton was workshopped at our very own Vassar College by Lin Manuel Miranda and is known as the Hamilton Mixtape! There is something for everyone here. Within a 30 minute drive you can explore the cities of Poughkeepsie, Beacon, New Paltz, Rhinebeck and Kingston; you can head to the surrounding suburbs to shop at the malls or local stores and enjoy activities like the hot air balloon festival, the Great Jack-O-Lantern Blaze or sunflower festival. You can participate in local farm shares or go horseback riding. For the ultimate city experience, we are only a 1.5 hour train ride along the picturesque Hudson River to get to New York City. It is nice to train in a place where you can see people as much or as little as you like during your time off.
How are you preparing your third-year residents for independent practice/applying for fellowship?
We want all of our graduates to have the freedom to pursue the career of their choosing. We meet with our residents who are interested in applying to fellowships and discuss the nuts and bolts of the process including a separate session on how to write a CV and another on how to ask for letters of recommendation and suggestions for interview days. We also provide our residents the opportunity to do a mock 1:1 interview with a faculty member. We also allow residents to do elective rotations elsewhere to explore programs which may be of interest to them in their fellowship pursuit. We have a curriculum for our residents on the business of medicine including coding and billing, evaluating opportunities in primary care and hospital medicine, navigating the recruiting process and what to look for in a contract.
We have added the Jr. Hospitalist (GRIT) and Jr. Primary Care Physician (GROT) rotations for all of our third-year residents. We understand that not everyone wants to be a hospitalist or a primary care doctor after graduation, but based on feedback from our graduates, regardless of career choice, the volume of patients cared for as an attending or a fellow is more demanding than what is often seen as a resident. We want to make sure that you feel confident that you can handle the increased intensity after graduation. We have a soft cap of 14 for the GRIT resident with the ability to flex up as the resident’s competence and comfort dictates. These rotations allow the senior resident to work 1:1 with an attending to really “try-on” the role of attending before graduation in a safe and supportive environment. It allows the resident to test their management plans and ensure that they are comprehensive while considering the personal preferences of the patient and any limitations due to insurance constraints. On the GROT rotation, again the resident works 1:1 with an attending to manage the complexities of outpatient medicine.
Will I be able to work with medical students?
Yes! We have rotating MS3 and MS4 from Touro School of Osteopathic Medicine in Middletown rotating on many of the medicine rotations. We also have some visiting students from other medical schools. There are PA students from Marist College as well as MS4s who rotate from other medical schools.
Do you have any rotations with 24-hour call?
No. We have a night float system both during medicine wards and ICU so that you never work a 24-hour shift.
What are the rules around vacation?
Residents have 4 weeks of vacation per year. In general, these weeks are broken down into 2 two-week blocks but on occasion can be taken as a 4-week block.
How do you support our success with the Internal Medicine Boards?
We want every resident in our program to pass the boards and are committed to giving you the best opportunity to do so. We have incorporated the ACP Board Review curriculum (residents all have access to the entire lecture series as well to review on their own) as the backbone of our noon conference didactics which incorporates board questions into the topic lectures. We also purchased the NEJM Knowledge+ question bank for all of the residents and assign weekly quizzes. Furthermore, each resident has a generous annual stipend to use for additional board materials. As described in our conference curriculum above, we have board review as part of noon conference and afternoon report which helps not only with topic review, but the approach to test questions and developing good test taking skills.
