Zucker School of Medicine at Hofstra/Northwell Internal Medicine Residency Program at Vassar Brothers Medical Center
A message from the Program Director
Dear Future Applicant,
Welcome, and thank you for considering the Internal Medicine Residency Program at Vassar Brothers Medical Center (VBMC), part of the Zucker School of Medicine at Hofstra/Northwell. As Program Director, I am honored to lead a program built on two core values: excellence in education and exceptional patient care. We are a young, innovative program that blends the expertise and success from our own diverse medical education training with the agility and curiosity to adapt and grow; a balance that helped us thrive through challenges like the pandemic.
Clinical Training in a Dynamic Environment
VBMC is a 350-bed tertiary care hospital in Poughkeepsie, NY, offering a rich clinical experience in a community setting. With 66 ER beds, 30 ICU beds, and over 2,000 monthly discharges, our residents encounter a wide range of pathology comparable to busy academic centers. Advanced procedures such as TAVR, ECMO, PCI, and EBUS are performed onsite, supported by all major subspecialties. All inpatient rotations take place at VBMC, ensuring continuity and depth in your clinical training.
Community, Wellness, and Support
Despite being a 75-resident program, we’ve intentionally cultivated a close-knit, supportive environment where lifelong friendships are formed. Our 4+1 schedule allows residents to bond deeply with their ambulatory cohort, sharing golden weekends every five weeks throughout all three years. We value your individuality and actively seek resident feedback to continuously improve the program. One of my greatest joys is hearing from graduates, whether it’s a professional milestone or a personal celebration, because we remain part of your journey long after residency.
Education and Career Development
Your education is our top priority. Residents benefit from protected learning time each weekday, including noon conferences, subspecialty small-group sessions, afternoon reports, and ambulatory academic half-days. Our advising program begins early in intern year, helping you explore diverse career paths (primary care, hospitalist medicine, or subspecialty fellowship), and tailor your journey without requiring early commitment to a formal track. As part of the Northwell GME network, you’ll also have access to global health opportunities, research through the Feinstein Institutes, and additional electives across a broad system.
Research, Growth, and What Comes Next
All residents participate in scholarly activity, with many presenting at national conferences such as ACP, SGIM, CHEST, ACC, AHA, ATS, and more. Our graduates have successfully gone on to careers in primary care, hospitalist medicine or a medical subspecialty. Residents have gone on to competitive fellowships, often earning chief fellow roles, national awards, and faculty appointments.
We hope you’ll choose to stay and join our medical community after graduation, but wherever your path leads, we’re here to support you in reaching your fullest potential. We invite you to apply and experience the professional growth and personal connection that define our program, all while enjoying the beauty of the Hudson Valley.
Looking forward to being part of your journey.
Sincerely,
Susan Collins, MD, FACP
Program Director
Zucker School of Medicine at Hofstra/Northwell
Internal Medicine Residency at
Vassar Brothers Medical Center
Program Structure
As an ACGME-accredited internal medicine residency program, our curriculum and clinical training experiences will prepare graduates to be not only independent practitioners or candidates for fellowship training, but also leaders in the field of medicine. By graduation, all residents will receive approximately the same exposure listed below in terms of weeks. The structure allows residents to develop a solid foundation in internal medicine with the flexibility to tailor your experiences as a second- and third-year resident to prepare you best for your future career choice.
PGY1
| 10-11 weeks | Ambulatory Medicine |
| 2-4 weeks | Medical Step-down Unit |
| 2-4 weeks | Inpatient Cardiology |
| 12-14 weeks | Inpatient Medicine |
| 4-6 weeks | Night Medicine |
| 8-10 weeks | Intensive Care Unit |
| 4 weeks | Emergency Medicine |
| 2 weeks | Ambulatory Selective |
| 2 weeks | Elective |
| 4 weeks | Vacation |
PGY2
| 10-11 weeks | Ambulatory Medicine |
| 8-10 weeks | Inpatient Medicine |
| 2-4 weeks | Inpatient Cardiology |
| 4-6 weeks | Night Medicine |
| 4-6 weeks | Intensive Care Unit |
| 2 weeks | Geriatrics |
| 2 weeks | Neurology |
| 2-4 weeks | PGY2 Jr. Hospitalist (Graduated Responsibility Inpatient Training aka PGY2 GRIT) |
| 12 weeks | Elective (including 2 weeks of ambulatory selective) |
| 4 weeks | Vacation |
PGY3
| 10-11 weeks | Ambulatory Medicine |
| 2-4 weeks | Jr. Primary Care Physician (Graduated Responsibility Outpatient training aka GROT)
Jr. Hospitalist (Graduated Responsibility Inpatient Training aka PGY3 GRIT) |
| 2-4 weeks | Medical Step-down Unit |
| 2 weeks | Quality (Quality, Leadership, Medical Education, Antibiotic Stewardship) |
| 6-8 weeks | Admitting Resident/Triage Resident/Consult Resident/Day Float |
| 2-4 weeks | Observation Rounder |
| 4-6 weeks | Intensive Care Unit |
| 4-6 weeks | Night Medicine |
| 11-12 weeks | Elective (including option to do 3 weeks of dedicated Point-of-Care Ultrasound training) |
| 4 weeks | Vacation |
The 4+1 Schedule
The Zucker School of Medicine at Hofstra/Northwell Internal Medicine Residency Program at Vassar Brothers Medical Center structure is a three-year program in which our residents usually spend 4 weeks on a given assignment (for example medicine wards or ICU), then one full week in the ambulatory setting which includes dedicated continuity clinic time to see an assigned patient panel. This 4+1 structure allows the resident to focus on learning from the rotation they are on at the time and gives protected time to the ambulatory experience to develop longitudinal relationships with patients.
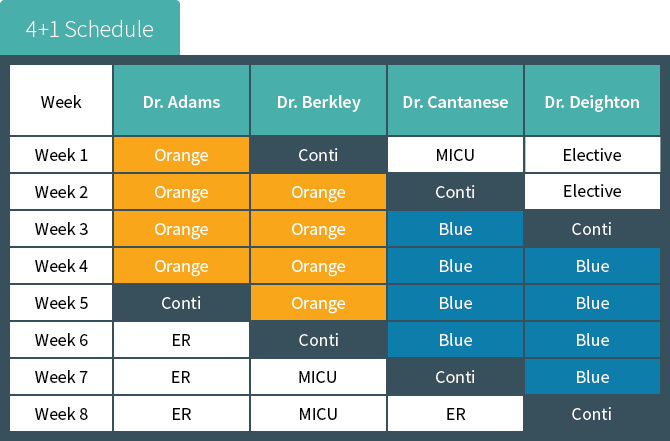
In the above example, Dr. Adams begins his academic year with a four-week rotation on the inpatient medicine orange team. When the fourth week is over, Dr. Adams spends one week rotating in the
continuity clinic and in various other internal medicine subspecialty clinics. Dr. Adams then changes to the next rotation, emergency medicine.
Note that as Dr. Adams is leaving the continuity clinic week, Dr. Berkley is coming into her continuity clinic week; and the pattern continues with Dr. Catanese and Dr. Deighton. These four individuals together comprise the continuity clinic “firm.”
Firms are an additional benefit to our program’s structure. Each firm’s cohort of residents acts as practice partners for one another, mimicking the structure of most private group practices. This real-world experience reinforces the skills and competencies required to be fully prepared to successfully practice medicine by the end of training. The Academic Practice Faculty are dedicated solely to the education of our residents and precepting their patients.
Our goal is to give our residents exposure to all the subspecialties with which a well-rounded primary care physician should be familiar. We have asked our subspecialty faculty to make sure that during the rotations the residents become familiar with common medical conditions in their field but also learn to identify the “red flag” things that would trigger a consult to a specialist on either a routine or urgent basis. In addition to seeing their own panel of patients in the Academic Practice, our interns spend time during the ambulatory week rotating through other medical and non-medical subspecialties to help inform their practice as primary care physicians (ie ophthalmology, physical therapy, infectious disease, etc). Our second- and third-year residents continue to manage their own panel of patients and establish an additional outpatient continuity clinic site either in a medicine subspecialty practice of their choosing or at another primary care site. Also, they have protected time during their ambulatory weeks to design, develop and implement their required scholarly project.
The Ambulatory Experience
Ambulatory Activities:
| Activity | Session(s) | Location |
| Continuity Clinic | 4-5 | P.C. Poughkeepsie Primary Care or Castle Point VA |
| Panel Management | 1 | P.C. Poughkeepsie Primary Care or Castle Point VA |
| Specialty Clinic and/or Scholarly Activity | 1-4 | Ophthalmology, Physical Therapy, IM Subspecialty Office |
| Academic Half Day | 1 | VBMC |
Continuity Clinic
P.C. Poughkeepsie Primary Care, a Northwell Health Medical Practice, is one of the continuity clinic sites for all our residents and is conveniently located adjacent to Vassar Brothers Medical Center. It is a fully academic primary care practice that serves a diverse population of patients in terms of demographics, socioeconomic status, ethnicity, language, and payer mix. At this office, every patient is scheduled to see a resident, great steps are taken to ensure continuity in patient care when scheduling appointments, and the wait time for appointments is usually short. Residents are encouraged to provide high value, high quality care and routinely perform appropriate ambulatory procedures for their panel of patients such as pelvic and breast exams as well as urgent procedures such as incisions and drainages, injections, and more. There is great emphasis placed on the importance of preventive medicine, patient education, communication skills, and patient and resident satisfaction. At this site, residents participate in in-office and telemedicine visits and second- and third-year residents take turns providing after-hours phone call coverage for patients of this office.
The other continuity clinic site is located in the Castle Point Veterans Affairs Hospital. The population of patients at this site tends to be older and more likely to be of male sex then our other continuity site; however, steps are taken to ensure the experience is comparable as residents are assigned to one or the other location based on their preferences and availabilities and not both. It should be noted, that second-year residents who have continuity clinic at the VA will spend one half-day per week in the Poughkeepsie office seeing patients with same day visits, those that require procedures, and those who need pre-operative or hospital discharge follow up visits. In addition, all third-year residents spend a dedicated 2 weeks at the Poughkeepsie office for the GROT (Graduated Responsibility in Outpatient Training) rotation.
Ambulatory Firms
Continuity is a key principle to successful patient care and, as such, we go to great lengths to ensure the patients are scheduled for their resident primary care providers for routine visits; however, residents are not always available to address their ambulatory patient’s needs. To ensure continuity in coverage, each resident is assigned to a firm of residents who provide coverage for unexpected patient issues that arise between regularly scheduled visits such as tasks and urgent appointments. Residents regularly communicate with members of their firm in-person and via our EMR to ensure their patients receive the best care no matter what rotation they are currently rotating on.
Specialty Clinic
Residents participate in high-yield specialty experiences guided by expert attending specialist providers throughout the Northwell Health network. While these experiences are assigned to interns, second- and third-year residents can choose their area of specialty in order to provide additional, focused training congruent with their future career goals. Interns will spend 3 half-days of their ambulatory week at the Ophthalmology, Infectious Disease, Warfarin Clinic, Hematology/Oncology, and Physical Therapy offices. Second- and third-year residents will spend a half day in a specialty office during their ambulatory weeks. They will be assigned to a specific office based on their preferences and availabilities as well as the availabilities of the offices.
Panel Management
Panel management is a proactive approach to healthcare delivery that aims to ensure that all patients of a given care team receive the necessary preventive services and chronic disease management they deserve, not just those who present for office visits. During the ambulatory week, each resident is given one session (during which they are not scheduled for patient visits) to review their panel of patients, conduct necessary outreach, and plan for in-reach at upcoming visits in order to provide better coordinated care, remain informed and engaged in their patients’ health, improve patients’ clinic outcomes while reducing healthcare costs, and increase the promotion of preventive medicine by closing care gaps identified. Patients and their resident primary care providers are encouraged to regularly communicate with each other via the patient portal.
Ambulatory Academic Half Day
Every Wednesday morning, residents on ambulatory week gather to participate in the Ambulatory Academic Half Day, which includes dedicated workshops, simulations, didactics, and case reviews. The designation of this time to educational endeavors ensures our residents get the highest quality education without the burden of conflicting responsibilities such as patient care and task completion. The weekly sessions include a workshop or simulation exercise, a didactic discussion, and participation in a case-based discussion of high-yield topics in ambulatory medicine as outlined in the Yale Curriculum under a central theme. For example, during the Diabetes Ambulatory Academic Half Day, residents participate in a workshop designed to teach them how to perform finger stick glucose measurements and administer insulin (using actual glucometers, insulin pens, and other supplies), discuss the American Diabetic Association guidelines for the pharmacologic treatment of type 2 diabetes guided by representative MKSAP questions, and complete the corresponding Yale Curriculum modules.
Conference Curriculum
Inpatient Medicine Afternoon Report
Afternoon Report is a case-based conference which allows residents and faculty to discuss patient care in an organized and efficient manner. Residents present cases to their peers and faculty with a faculty member as the facilitator. The facilitator uses the information in the resident’s presentation as a springboard for robust conversation and discussion to develop medical knowledge and critical thinking skills with a focus on evidence-based practice and high-value care. Interns and residents have separate afternoon report conferences to focus on level-appropriate aspects of diagnosis and management. Resident report is Monday and Intern report is every Friday while the resident is on medicine wards. Board review is done every Wednesday afternoon for residents on the wards where a resident is assigned to put board review questions into a fun “Jeopardy” game format.
Subspecialty Teaching
On Tuesday and Thursday mornings during inpatient wards, the ward team meets in small groups of around 6 residents with a subspecialist attending who does a small group “chalk talk.” This is a revolving curriculum so that by the end of residency all the residents have participated in these sessions. These sessions not only allow the residents to learn skills best taught in such an environment like interpretation of EKGs or understanding non-invasive ventilation options, but it also gives you unique access to subspecialty attendings which naturally fosters collegiality and mentorship which is essential for collaboration in the future on scholarly activity or possibly fellowship pursuit. Current subspecialty teaching sessions include gastroenterology, cardiology, pulmonary, infectious disease, rheumatology, nephrology and hematology/oncology. It is a wonderful opportunity – it is not unusual to see a BIPAP machine being wheeled down the hall by the pulmonologist to have the residents learn how to set it up and what the mask feels like.
Noon Conference Series
Our Internal Medicine Noon Conference Curriculum is the core of our academic and didactic series. It occurs Monday thru Friday each week. Taught by board-certified internists and subspecialists, the curriculum is designed to provide residents with a wealth of topics and cases that span the care continuum. We have introduced the ACP Board Review Curriculum as the backbone of our didactics for academic year 2025-2026. We integrate didactics as well as team-based learning exercises to try and meet the needs of our learners. To maximize the experience, Dr. Collins sends out a weekly email with the noon conference topics for the following week along with the recommended reading either from primary articles, review articles or from AMBOSS/NEJM Resident 360. The IM Chiefs send a “Weekly Digest E-mail” to go over what was covered throughout the week with a focus on practicing current guidelines and board review. Board review questions are assigned throughout the year in AMBOSS related to the topics reviewed.
Other regular conferences topics include high-value care, health care disparities, the business of medicine, career development (“Prepare to Launch” series by Dr. Feldberg, Associate Program Director), resident as teacher and wellness. The “Achieving ROSC (Reinforcing Our Specialty Core) Series” was developed this year and consists of senior resident run lectures with faculty support. The objective is to present high-yield topics in IM to refresh our knowledge with the opportunity to present new practice changes/findings.
Internal Medicine Grand Rounds
Grand Rounds conference is a platform for faculty and invited speakers to present on a variety of topics, including case-based presentations, research, or current relevant topics in the field of Internal Medicine. Grand Rounds occurs monthly during noon conference.
Serious Event Analysis (SEA)
Serious event analysis/Quality and Process Improvement, formerly Mortality and Morbidity (M&M), occur monthly and are presented by residents with a faculty mentors’ guidance. They are joint conferences with critical care as well as other specialties. Topics are decided by residents and faculty based on actual patient care cases where a significant system error occurred. SEA provides a forum for resident interaction and discussion with attending physicians regarding care that could have been improved, and the opportunity to identify system errors. The faculty mentors facilitate the discussion based on the topic with a focus on approach to root cause analysis.
Residents’ Journal Club
As a first step in learning how to effectively practice evidence-based medicine, interns and residents participate in a weekly Journal Club to appraise a recent study published in the medical literature. Each intern presents at least once at Journal Club. They partner with a subspecialist/internist for development of the topic review and with our Associate Program Director, Dr. Valerie Cluzet, to critically appraise the study, and then presents the appraisal to their peers and faculty during noon conference.
Board Review
Board review is incorporated into noon conference as part of the ACP curriculum as well as into weekly medical knowledge “Jeopardy” games on Wednesday afternoons. Additionally, residents are provided with access to AMBOSS.
Joint Program Lecture Series
The lecture series covers GME-wide topics such as resident fatigue, burnout, resident wellness and other issues. Sessions will be hosted by the GME office and invited speakers will present. Topics include, but are not limited to:
- Fatigue
- Stress and depression
- Substance abuse
- Disruptive behavior
- Burnout
- Boundary violations
- Impairment
- Instructive feedback
ABIM In-Service Training Exam
Residents’ medical knowledge and clinical reasoning is benchmarked for measuring longitudinal growth through the results of the annual American Board of Internal Medicine In-Service Training Examination. All internal medicine residents complete the exam annually. Results are reviewed individually with the program director to inform discussions and individualization of curriculum and clinical training (e.g., reading material, board prep and electives). Struggling learners work closely with program leadership to improve study habits and test taking skills so that their confidence improves over the three years well in advance of the actual board exam.
Academic Half Day
Every Wednesday morning, residents on ambulatory week gather to participate in the Ambulatory Academic Half Day, which includes dedicated workshops, simulation, didactics, and case reviews. See Ambulatory Experience tab for further details.
Point-of-Care Ultrasound (POCUS)
POCUS is incorporated into our simulation training, didactics, electives and clinical practice.
Narrative Medicine Curriculum
Dr. Christine Kerr has introduced a narrative medicine curriculum for all our residents to participate in during small group sessions. This is a unique opportunity to share experiences and develop skills to help process these events as an active way to combat burnout in medicine. Int J Psychiatry Med. 2020 Sep;55(5):321-330.
Research and Quality Improvement Opportunities
Scholarly Activity Program
The goal of the internal medicine scholarly activity curriculum is to advance each resident’s knowledge of the basic principles of epidemiology and clinical research, including how it is conducted, evaluated, explained to patients, and applied to patient care. Understanding and appraisal of the medical literature is critical to providing evidence-based care. In addition to weekly Journal Club, with discussion of critical appraisal of the medical literature (see Conference Curriculum), all residents in the Program are provided opportunity for, and are fully supported in scholarly activity, including research, quality improvement (QI) and medical education pursuits.
We require each resident to complete scholarly activity and protected time is allotted during ambulatory weeks to work on the projects for the duration of the residency. There is a point system whereby points are earned based on the type of scholarly activity and 10 points are required to graduate.
Examples of scholarly activity include research studies, case reports or case abstracts, quality improvement projects, teaching presentations, etc. Additional participation by residents above the minimum requirements are typical and highly encouraged. Dr. Valerie Cluzet, Associate Program Director, mentors all residents in the development and conduct of scholarly activity projects that reflect each resident’s interests and career goals. Elective time to work on scholarly activities is also available, with rotation-specific curriculum outlining the goals and objectives, requirements, and expectations for the rotation. In addition to individual scholarly projects, all residents will be coached in approach to QI and participate in a group QI project (see Quality Improvement Curriculum below).
As of end of academic year 2024-2025, the PGY2 and PGY3 residents had 49 research abstracts and 90 clinical vignettes accepted for presentation at national and regional conferences, 10 case reports and 22 review articles accepted for publication in peer-reviewed journals and completed 6 QI projects. Other scholarly projects include curriculum development, teaching presentations and education to the public.
The Research Department also offers a trainee track for their Research Academy, where participating residents are offered lectures and workshops on clinical research and have mentorship to develop an original research protocol and lead a research project to completion. Dr. Cluzet serves as a mentor for the Research Academy. Currently, 5 residents from the VBMC IM Program participate.
Quality Improvement Activities
Our “Quality Time with the Residents” program introduces residents in their intern year to Quality Improvement and Patient Safety. During their ambulatory weeks, interns meet with Dr. Collins and Dr. Webb as well as Quality Department leadership. They learn how to develop a quality improvement project in a step wise process. They work in small groups along with a core faculty member to design a project, implement an intervention and measure the effectiveness of the intervention. Our goal is to empower our learners to understand the important role they play in improving the quality of care and patient safety. They are encouraged to disseminate their work in local, regional and national conferences.
Application Process
The Zucker School of Medicine at Hofstra/Northwell Internal Medicine Residency Program at Vassar Brothers Medical Center (ACGME ID # 1403500932) thanks you for your interest in applying to our program. We are an ACGME accredited internal medicine residency program. We accept applications through ERAS only and participate annually in the NRMP Match (NRMP #: 2495140C0) Program.
Please note: For International Medical Graduate applicants, only J1 visas are considered at this time.
Signaling: While we preferentially review applications from those who signal our program, we also consider applicants who do not signal us.
Requirements: The following items are required for consideration of interview. All items must be received through ERAS application portal:
- Personal Statement
- Current CV
- 3 Letters of Recommendation
- USMLE Step 1 Pass or COMLEX Level 1 Score
- USMLE Step 2 CK or COMLEX Level 2 CE Score
- MSPE (Dean’s) Letter
Timeline: We will interview candidates during select dates in November, December and January. Exact dates will be provided to the invited residency applicants via email notification.
Please note, New York State has a 12-week rule for graduates from a non-LCME-accredited medical school regarding limiting the number of required clerkships during medical school that are performed outside of the country of training. See https://www.op.nysed.gov/professions/physicians/license-requirements for further information.
Interviewing
After reviewing applications in ERAS we will send out invites via e-mail with available dates for interviewing. All interviews will be done virtually for the 2026 interview season.
What to expect for the interview day? We do our interviews via Thalamus. You will meet with Dr. Susan Collins the Program Director for an overview of the program. and you will have three faculty interviews. You will also spend time with our program managers learning more about the area and the benefits of training at Vassar Brothers Medical Center. Most importantly, you will spend time with our current residents in breakout sessions where you can ask them all about the area, the program and why they chose to train here. You will also be invited to meet with our chief residents and residents during evening meet and greets during interview season and join some of our noon conferences.
Post-interview communication: We are available for any questions that may arise after your interview day. Please free to reach out to the Program Managers: Nancy Hebrank, Alexandra Belmonte and Christopher Santiago at VBMCIMRecruitment@nuvancehealth.org and to the Chief Residents at VBMCInternalMedicineChiefs@nuvancehealth.onmicrosoft.com if you have any lingering questions during this often chaotic time. Please do not feel obligated in any way to provide a thank you note to any of our faculty. Our policy is to not provide any communication to you regarding ranking, fit or preference.
Wellness
We have our own Internal Medicine Residency Wellness Committee to support wellness activities. Previously our residents have participated in team building activities such as: mini-golfing, bowling, painting night, Lego building competitions, movie watch parties, game nights and so much more.
We have monthly noon conferences dedicated to wellness, organized by the wellness committee leadership.
We have a narrative medicine curriculum to address the feelings and experiences that occur when caring for the ill.
We also ensure that our residents average weekly duty hours are well under 80 hours by creating a schedule and admitting cap to allow residents adequate time off to focus on developing a work-life balance.
The program organizes an annual wellness retreat for our Internal Medicine residents to enjoy!
Our Graduates
Graduate Class of 2025
Fellowship (10)
- Allergy and Immunology (1)
- Cardiology (1)
- Endocrinology (4)
- Infectious Diseases (1)
- Pulmonary and Critical Care (3)
Hospitalist (10)
Primary Care (6)
Graduate Class of 2024
Fellowship (13)
- Cardiology (1)
- Endocrinology (1)
- Hematology and Oncology (2)
- Hospice and Palliative Medicine (1)
- Nephrology (1)
- Hospice and Palliative Medicine (1)
- Pulmonary and Critical Care (5)
- Rheumatology (1)
Hospitalist (11)
Graduate Class of 2023
Fellowship (12)
- Advanced Heart Failure and Transplant (1)
- Cardiology (1)
- Endocrine (1)
- Hematology and Oncology (2)
- Hospice and Palliative Medicine (1)
- Infectious Disease (1)
- Pulmonary and Critical Care (3)
- Rheumatology (2)
Hospitalist (10)
Primary Care (3)
Graduate Class of 2022
Fellowship (14)
- Critical Care (1)
- Endocrinology (1)
- Hematology/Oncology (1)
- Infectious Disease (2)
- Medical Genetics (1)
- Medical Oncology (1)
- Nephrology (3)
- Pulmonary Critical Care (2)
- Rheumatology (2)
Hospitalist (9)
Primary Care (2)
Our Mission
Our overall two main drivers are to provide phenomenal patient care and to pursue excellence in education. As a program our aim is to build better health for our community by training leaders in the delivery of high quality, compassionate healthcare for a community rich in cultural, economic, gender, racial and physical diversity.
Fast Facts
PROGRAM HIGHLIGHTS
- A “4+1” training model that allows residents to spend one week fully dedicated to continuity of care for their primary care patients in between four-week blocks assigned to a given rotation
- Team-based training with direct patient care and progressive responsibility as residents advance through the program
- Diverse training program with specialty experiences in neurology, critical care, cardiology, endocrinology, pulmonary medicine, geriatrics, rheumatology, point-of-care ultrasound, palliative care and more.
- Daily didactic training exploring topics such as basic sciences, clinical practice, medical ethics and research methods
- Committed, passionate, diverse faculty
- A mentorship program to facilitate professional and personal growth and provide support throughout training
- All residents participate in scholarly activity and/or quality improvement projects
- Emphasis on resident well being
- All residents participate in scholarly activity and/or quality improvement and often present at national conferences
During the first year of training, interns care for patients in the emergency department, ICU and medical floors at Vassar Brothers Medical Center, a large tertiary care facility with high patient acuity. They begin to build their panel of patients in their continuity clinic where they will care for the patients over the next 3 years. They will work directly with a co-intern, a senior resident and attending physician. Each intern will present at journal club and participate in the Quality Time with the Residents curriculum to design and implement a quality improvement project.
During the second year of training, residents will gain experience leading the medical team under the close supervision of their attending physician as they have progressively more independence. Residents gain more confidence and have elective time to explore possible career paths.
During the third year of training, residents will gain progressive independence and will solidify their clinical knowledge in more challenging roles with triage and consults developing leadership skills and increased patient care responsibilities. Third-year residents take the lead on cases, and will act as clinicians, leaders and teachers. Third-year residents will also have several elective opportunities to guide their own training path and prepare for the next stage of their career.
FAQs
Why should I come to the Hudson Valley for residency?
It’s beautiful here! It is lovely to enjoy four seasons with apple-picking and hiking with brilliant, colorful foliage in the fall; skiing, sledding, snowboarding and ice skating in the winter; more kayaking and biking in the spring, and enjoying swimming, outdoor concerts, drive-in movie theaters, water parks and more in the summer. We have fantastic restaurants with the Culinary Institute of America 10 minutes away from the hospital and we benefit from a lot of their graduates settling locally. We have multiple local colleges and universities which provide an array of cultural opportunities – the initial Hamilton was workshopped at our very own Vassar College by Lin Manuel Miranda and is known as the Hamilton Mixtape! There is something for everyone here. Within a 30 minute drive you can explore the cities of Poughkeepsie, Beacon, New Paltz, Rhinebeck and Kingston; you can head to the surrounding suburbs to shop at the malls or local stores and enjoy activities like the hot air balloon festival, the Great Jack-O-Lantern Blaze or sunflower festival. You can participate in local farm shares or go horseback riding. For the ultimate city experience, we are only a 1.5 hour train ride along the picturesque Hudson River to get to New York City. It is nice to train in a place where you can see people as much or as little as you like during your time off.
How are you preparing your third-year residents for independent practice/applying for fellowship?
We want all of our graduates to have the freedom to pursue the career of their choosing. We meet with our residents who are interested in applying to fellowships and discuss the nuts and bolts of the process including a separate session on how to write a CV and another on how to ask for letters of recommendation and suggestions for interview days. We also provide our residents the opportunity to do a mock 1:1 interview with a faculty member. We also allow residents to do elective rotations elsewhere to explore programs which may be of interest to them in their fellowship pursuit. We have a curriculum for our residents on the business of medicine including coding and billing, evaluating opportunities in primary care and hospital medicine, navigating the recruiting process and what to look for in a contract.
We have added the Jr. Hospitalist (GRIT) rotation for all of our third-year residents. We understand that not everyone wants to be a hospitalist after graduation, but based on feedback from our graduates, regardless of career choice, the volume of patients cared for as an attending or a fellow is more demanding than what is often seen as a resident. We want to make sure that you feel confident that you can handle the increased intensity after graduation. We have a soft cap of 14 for the GRIT resident with the ability to flex up as the resident’s competence and comfort dictates. These rotations allow the senior resident to work 1:1 with an attending to really “try-on” the role of attending before graduation in a safe and supportive environment. It allows the resident to test their management plans and ensure that they are comprehensive while considering the personal preferences of the patient and any limitations due to insurance constraints. We have similar outpatient elective experiences available for residents who plan to pursue a career in primary care (GROT).
Will I be able to work with medical students?
Yes! We have rotating MS3 and MS4 from Touro School of Osteopathic Medicine in Middletown rotating on many of the medicine rotations. We also have some visiting students from other medical schools. There are PA students from Marist College as well as MS4s who rotate from other medical schools.
Do you have any rotations with 24-hour call?
No. We have a night float system both during medicine wards and ICU so that you never work a 24-hour shift.
What are the rules around vacation?
Residents have 4 weeks of vacation per year. In general, these weeks are broken down into 2 two-week blocks but on occasion can be taken as a 4-week block.
How do you support our success with the Internal Medicine Boards?
We want every resident in our program to pass the boards and are committed to giving you the best opportunity to do so. We have incorporated the ACP Board Review curriculum (residents all have access to the entire lecture series as well to review on their own) as the backbone of our noon conference didactics which incorporates board questions into the topic lectures. We also purchased the NEJM Knowledge+ question bank for all of the residents and assign weekly quizzes. Furthermore, each resident has a generous annual stipend to use for additional board materials. As described in our conference curriculum above, we have board review as part of noon conference and afternoon report which helps not only with topic review, but the approach to test questions and developing good test taking skills.
