Resident Reflections

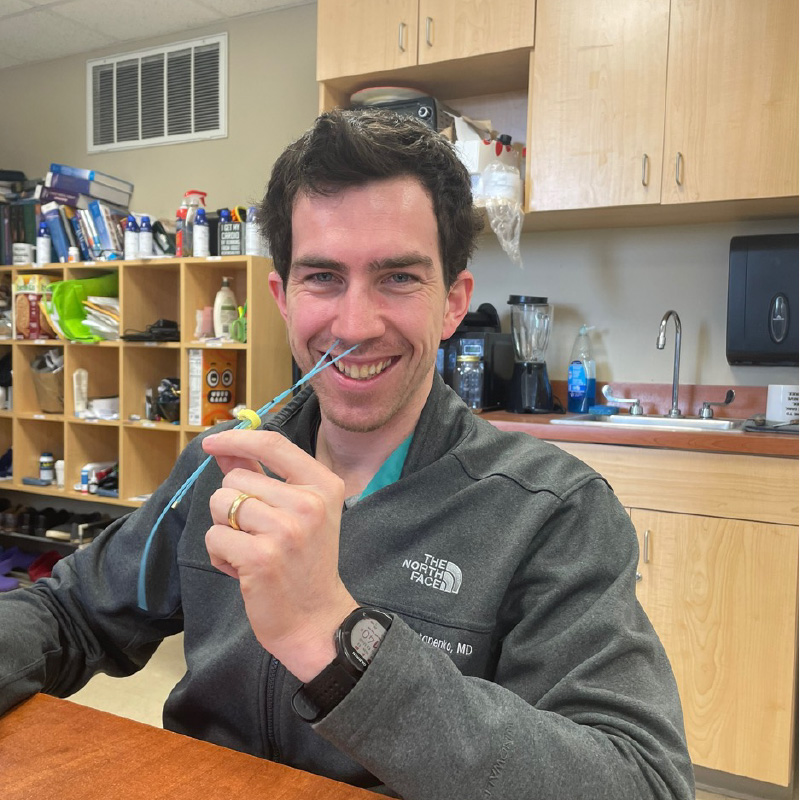
Krist Aploks, M.D.
PGY 5
I was originally attracted to Danbury for both its stellar academic reputation and its tight-knit community setting. I feel like I get great exposure to a wide variety of surgical pathology, yet still know everyone’s name at the end of the day. What has kept me here, however, is the support that I get from my fellow residents. We have a great group that really looks out for each other, both in and out of the hospital. Even after spending 20+ hours together during the week, we still find time to grab a meal or a drink together post-call. I feel like that’s something you don’t find everywhere, and honestly it makes me excited to come to work every day.

Natasha Sebastian, M.D.
PGY 4
I chose Danbury Hospital because it provides a large residency volume in a community setting. Choosing a community residency program offers a unique blend of diverse patient populations, hands-on surgical experience, and close mentorship from seasoned surgeons. I value the opportunity to make a direct impact on my community’s health while developing a broad skill set that prepares me for a versatile surgical career. Additionally, the collaborative environment and emphasis on continuity of care align perfectly with my professional goals of becoming a proficient and compassionate surgeon.
 Keerthivasan Vengatesan, M.D
Keerthivasan Vengatesan, M.D
PGY 3
Danbury Hospital felt like the perfect hybrid of academic opportunities and community-focused care. The camaraderie among the residents and between the residents and faculty really stood out to me. Residents get access to significant OR and bedside procedure experience as early as intern year, there is a significant focus on resident education and simulation, and the leadership really strives to help us achieve our personal goals.

Sidney Smilen, D.O.
PGY 2
I chose Danbury Hospital for the individualized attention the the residents receive, including early operating experience and critical care management. The program’s size allows the faculty to develop relationships with the residents and accommodate to their learning styles. After my interview, it was clear to me the supportive and collaborative atmosphere that existed not only between the residents but the attendings as well.

Vasalya Panchumarthi, M.D.
PGY 1
I have felt extremely supported since beginning my residency at Danbury Hospital. The faculty are truly committed to resident success and work hard to provide us with the support and mentorship we need. There is a strong sense of camaraderie among the residents where we can joke and work as a team. I am extremely grateful being in a program that promotes well-being alongside learning.
Day in the life of a resident
- 5am: Wake up, get ready and head to work
- 5:30am: I get to the resident work-room and chart review all of the patients with regards to vitals,
ins/outs, labs, and any notable overnight events. I also read up on any new admissions or consults
overnight (if there are any) - 6am: We receive sign-out from the overnight team and then proceed with morning rounds, where the
resident team (including the chief, myself, the intern, and medical students) efficiently sees all of our
patients and checks in regarding any issues they had overnight and their progress - 7am: We briefly “run the list” (which is going over each patient and quickly discussing our plans for the
day for each). We then call the attendings and go over their specific patients in detail to solidify the
plans for those patients. We also split up notes to write as a team and ensure that any low electrolytes
are replaced - 7:15am: After rounds we then split off for our respective duties, for the chief and midlevel residents,
this often is operative cases for the day. The interns also get to operate however also focus on enacting
all the discussed plans. I see that I have 2 colectomies today. As I head to the pre-operative holding area
I recall the anatomy, steps of the operation, and any useful advice I’ve picked up from prior cases. I
introduce myself to the first patient in the holding area and quickly go over what their day is going to
look like with regards to the operation. I then head over to the OR we’ll be in and check in with the staff
there. Usually at this time I also give the scrub tech my sterile gown and gloves for the case - 7:30am: The case is underway! The attending and I go over each of the steps as we perform them as
well as review relevant anatomy that we see and tips and tricks for the next time. - 11am: After the first case ends, I write the appropriate post-operative orders and brief operative note
detailing what we did. Often the attending also rounds on his/her patients between cases so I
accompany them for rounds at this time. I then check in with the team to sign out the patient I just
operated on, as well as for any updates and to see how the plans are going and if any help is needed.
Thankfully, all is under control. I still have 10-15 minutes before my next case soI decide to grab a quick
bite to eat as I know the next case will also last a few hours and I don’t want to feel hungry during it.
Lunchtime can often vary during the day depending on the timing of the cases that are going. I feel that
it’s always better to eat something when you can. I then head back to the OR for the next case. - 3pm: After the second case ends, I check back in with the team to run the list again to ensure that all
the plans were completed during the day and help out where it is needed. We also ensure the list is
updated for the evening team, and that the patients all have the relevant labs ordered for the morning. - 5pm: We sign out to the overnight float team regarding our patients and pertinent issues to follow-up
on or be aware of overnight. I then head home for the day! - 5:30pm – 10pm: Every night I make sure that I prepare for and read up on my cases for the following
day and do some general studying. All this together takes up about 1-2 hours of my evening. The other
time is my own! Some of the activities I do on various evenings include going to the gym, hanging out
with my co-residents outside of work, making dinner, watching TV - 10pm: Bedtime!
Resident Life